Ubiquitin specific peptidase 18 (USP18), also known as UBP43, is a type I interferon receptor repressor and an isopeptidase. In humans, it is encoded by the USP18 gene.[5] USP18 is induced by the immune response to type I and III interferons, and serves as a negative regulator of type I interferon, but not type III interferon. Loss of USP18 results in increased responsiveness to type I interferons and life-threatening autoinflammatory disease in humans due to the negative regulatory function of USP18 in interferon signal transduction. Independent of this activity, USP18 is also a member of the deubiquitinating protease family of enzymes. It is known to remove ISG15 conjugates from a broad range of protein substrates, a process known as deISGylation.[5]
| USP18 | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | USP18, ISG43, UBP43, ubiquitin specific peptidase 18, PTORCH2 | ||||||||||||||||||||||||||||||||||||||||||||||||||
| External IDs | OMIM: 607057; MGI: 1344364; HomoloGene: 8047; GeneCards: USP18; OMA:USP18 - orthologs | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
Structure
editThe USP18 gene consists of 11 exons that encode a 43 kDa protein. The USP18 protein adopts the characteristic hand-like structure of ubiquitin-specific-proteases (USPs), which consists of a finger, palm and thumb domain. At the interface of the palm and thumb domain lies the catalytic site composed of the cysteine protease triad (cysteine, a histidine and an aspartate or asparagine).[6] The C-terminus of USP18 is primarily responsible for negative regulation of interferon-I signaling.[7]
Function
editFollowing its induction by type I interferons (IFN-Is), USP18 carries out three functional interactions:
Regulation of IFN-I signaling
editUSP18 inhibits IFN-I signaling by disrupting the receptor complex and the subsequent JAK-STAT signaling pathway. USP18 binds the IFN-receptor 2 subunit (IFNAR2), leading to the displacement of Janus kinase 1.[7][8] and the dissociation of the cytokine-receptor complex.[9] This process requires STAT2 to traffic USP18 to the receptor [10][11][12] These events terminate signaling and draw cells into a refractory state with diminished sensitivity to future stimulation.[8]
deISGylation
editUsing the isopeptidase domain, USP18 specifically deconjugates ISG15 (interferon-stimulated gene 15) from tagged proteins.[13] This reaction is termed deISGylation, as the initial conjugation of ISG15 to newly synthesized proteins is termed ISGylation, a process akin to ubiquitination. However, unlike other de-ubiquitinating enzymes, USP18 is specific to ISG15, and exhibits no cross-reactivity with ubiquitin. The consequences of ISGylation and deISGylation are incompletely understood.[14]
Stabilization
editUSP18 is stabilized by ISG15, but independently of the ubiquitin-like conjugation.[15] Without ISG15-mediated stabilization, USP18 is degraded at the proteasome. This relationship exists in human, canine and porcine USP18/ISG15,[16] but is absent in murine systems.[17]
Promoting factor of HIV infection
editMacrophages and dendritic cells are usually the first point of contact with pathogens, including lentiviruses. Host restriction factors, including SAMHD1, mediate the innate immune response against these viruses. However, HIV-1 has evolved to circumvent the innate immune response and establishes disseminated infection. It was reported that human USP18 is a novel factor potentially contributing to HIV replication by blocking the antiviral function of p21 in differentiated human myeloid cells. USP18 downregulates p21 protein expression, which correlates with upregulated intracellular dNTP levels and the antiviral inactive form of SAMHD1. Depletion of USP18 stabilizes p21 protein expression, which correlates with dephosphorylated SAMHD1 and a block to HIV-1 replication.[18][19][20][21][22]
Clinical significance
editUSP18-deficiency is a very rare primary immunodeficiency caused by mutations of the USP18 gene. The inheritance is autosomal recessive. The clinical disease presents in the perinatal period with life-threatening autoinflammation that mimics TORCH infections, but in the absence of infection. The severe inflammation results from a failure to regulate type I IFN activity, and is therefore considered a type I interferonopathy. This syndrome was initially described to result in death within weeks of birth.[23] Fortunately, this previously lethal condition was recently demonstrated to be curable with a Janus kinase inhibitor and intensive supportive care.[24]
References
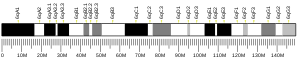
edit- ^ a b c GRCh38: Ensembl release 89: ENSG00000184979 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000030107 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ a b "Entrez Gene: USP18 ubiquitin specific peptidase 18".
- ^ Basters A, Knobeloch KP, Fritz G (December 2018). "USP18 - a multifunctional component in the interferon response". Bioscience Reports. 38 (6). doi:10.1042/BSR20180250. PMC 6240716. PMID 30126853.
- ^ a b Malakhova OA, Kim KI, Luo JK, Zou W, Kumar KG, Fuchs SY, et al. (June 2006). "UBP43 is a novel regulator of interferon signaling independent of its ISG15 isopeptidase activity". The EMBO Journal. 25 (11): 2358–67. doi:10.1038/sj.emboj.7601149. PMC 1478183. PMID 16710296.
- ^ a b François-Newton V, Magno de Freitas Almeida G, Payelle-Brogard B, Monneron D, Pichard-Garcia L, Piehler J, et al. (2011). "USP18-based negative feedback control is induced by type I and type III interferons and specifically inactivates interferon α response". PLOS ONE. 6 (7): e22200. Bibcode:2011PLoSO...622200F. doi:10.1371/journal.pone.0022200. PMC 3136508. PMID 21779393.
- ^ Wilmes S, Beutel O, Li Z, Francois-Newton V, Richter CP, Janning D, et al. (May 2015). "Receptor dimerization dynamics as a regulatory valve for plasticity of type I interferon signaling". The Journal of Cell Biology. 209 (4): 579–93. doi:10.1083/jcb.201412049. PMC 4442803. PMID 26008745.
- ^ Arimoto KI, Löchte S, Stoner SA, Burkart C, Zhang Y, Miyauchi S, et al. (March 2017). "STAT2 is an essential adaptor in USP18-mediated suppression of type I interferon signaling". Nature Structural & Molecular Biology. 24 (3): 279–289. doi:10.1038/nsmb.3378. PMC 5365074. PMID 28165510.
- ^ Gruber C, Martin-Fernandez M, Ailal F, Qiu X, Taft J, Altman J, et al. (May 2020). "Homozygous STAT2 gain-of-function mutation by loss of USP18 activity in a patient with type I interferonopathy". The Journal of Experimental Medicine. 217 (5). doi:10.1084/jem.20192319. PMC 7201920. PMID 32092142.
- ^ Duncan CJ, Thompson BJ, Chen R, Rice GI, Gothe F, Young DF, et al. (December 2019). "Severe type I interferonopathy and unrestrained interferon signaling due to a homozygous germline mutation in STAT2". Science Immunology. 4 (42): eaav7501. doi:10.1126/sciimmunol.aav7501. hdl:20.500.11820/3908eba0-5d5c-404d-b79f-08e6bd93b61d. PMC 7115903. PMID 31836668.
- ^ Malakhov MP, Malakhova OA, Kim KI, Ritchie KJ, Zhang DE (March 2002). "UBP43 (USP18) specifically removes ISG15 from conjugated proteins". The Journal of Biological Chemistry. 277 (12): 9976–81. doi:10.1074/jbc.M109078200. PMID 11788588.
- ^ Hermann M, Bogunovic D (February 2017). "ISG15: In Sickness and in Health". Trends in Immunology. 38 (2): 79–93. doi:10.1016/j.it.2016.11.001. PMID 27887993.
- ^ Zhang X, Bogunovic D, Payelle-Brogard B, Francois-Newton V, Speer SD, Yuan C, et al. (January 2015). "Human intracellular ISG15 prevents interferon-α/β over-amplification and auto-inflammation". Nature. 517 (7532): 89–93. Bibcode:2015Natur.517...89Z. doi:10.1038/nature13801. PMC 4303590. PMID 25307056.
- ^ Qiu X, Taft J, Bogunovic D (March 2020). "Developing Broad-Spectrum Antivirals Using Porcine and Rhesus Macaque Models". The Journal of Infectious Diseases. 221 (6): 890–894. doi:10.1093/infdis/jiz549. PMC 7050986. PMID 31637432.
- ^ Speer SD, Li Z, Buta S, Payelle-Brogard B, Qian L, Vigant F, et al. (May 2016). "ISG15 deficiency and increased viral resistance in humans but not mice". Nature Communications. 7: 11496. Bibcode:2016NatCo...711496S. doi:10.1038/ncomms11496. PMC 4873964. PMID 27193971.
- ^ Osei Kuffour, Edmund; Schott, Kerstin; Jaguva Vasudevan, Ananda Ayyappan; Holler, Jessica; Schulz, Wolfgang A.; Lang, Philipp A.; Lang, Karl S.; Kim, Baek; Häussinger, Dieter; König, Renate; Münk, Carsten (2018-10-15). Sundquist, Wesley I. (ed.). "USP18 (UBP43) Abrogates p21-Mediated Inhibition of HIV-1". Journal of Virology. 92 (20). doi:10.1128/JVI.00592-18. ISSN 0022-538X. PMC 6158439. PMID 30068654.
- ^ Chintala, Kumaraswami; Mohareer, Krishnaveni; Banerjee, Sharmistha (2021-07-29). "Dodging the Host Interferon-Stimulated Gene Mediated Innate Immunity by HIV-1: A Brief Update on Intrinsic Mechanisms and Counter-Mechanisms". Frontiers in Immunology. 12: 716927. doi:10.3389/fimmu.2021.716927. ISSN 1664-3224. PMC 8358655. PMID 34394123.
- ^ Gao, Wenying; Rui, Yajuan; Li, Guangquan; Zhai, Chenyang; Su, Jiaming; Liu, Han; Zheng, Wenwen; Zheng, Baisong; Zhang, Wenyan; Yang, Yongjun; Hua, Shucheng (2021-09-22). "Specific Deubiquitinating Enzymes Promote Host Restriction Factors Against HIV/SIV Viruses". Frontiers in Immunology. 12: 740713. doi:10.3389/fimmu.2021.740713. ISSN 1664-3224. PMC 8492978. PMID 34630422.
- ^ Rojas, Masyelly; Luz-Crawford, Patricia; Soto-Rifo, Ricardo; Reyes-Cerpa, Sebastián; Toro-Ascuy, Daniela (2021-09-09). "The Landscape of IFN/ISG Signaling in HIV-1-Infected Macrophages and Its Possible Role in the HIV-1 Latency". Cells. 10 (9): 2378. doi:10.3390/cells10092378. ISSN 2073-4409. PMC 8467246. PMID 34572027.
- ^ Sugawara, Sho; El-Diwany, Ramy; Cohen, Laura K.; Rousseau, Kimberly E.; Williams, Christopher Y. K.; Veenhuis, Rebecca T.; Mehta, Shruti H.; Blankson, Joel N.; Thomas, David L.; Cox, Andrea L.; Balagopal, Ashwin (2021-04-26). Simon, Viviana (ed.). "People with HIV-1 Demonstrate Type 1 Interferon Refractoriness Associated with Upregulated USP18". Journal of Virology. 95 (10). doi:10.1128/JVI.01777-20. ISSN 0022-538X. PMC 8139647. PMID 33658340.
- ^ Meuwissen ME, Schot R, Buta S, Oudesluijs G, Tinschert S, Speer SD, et al. (June 2016). "Human USP18 deficiency underlies type 1 interferonopathy leading to severe pseudo-TORCH syndrome". The Journal of Experimental Medicine. 213 (7): 1163–74. doi:10.1084/jem.20151529. PMC 4925017. PMID 27325888.
- ^ Alsohime F, Martin-Fernandez M, Temsah MH, Alabdulhafid M, Le Voyer T, Alghamdi M, et al. (January 2020). "JAK Inhibitor Therapy in a Child with Inherited USP18 Deficiency". The New England Journal of Medicine. 382 (3): 256–265. doi:10.1056/NEJMoa1905633. PMC 7155173. PMID 31940699.
Further reading
edit- Li XL, Blackford JA, Judge CS, Liu M, Xiao W, Kalvakolanu DV, Hassel BA (March 2000). "RNase-L-dependent destabilization of interferon-induced mRNAs. A role for the 2-5A system in attenuation of the interferon response". The Journal of Biological Chemistry. 275 (12): 8880–8. doi:10.1074/jbc.275.12.8880. PMID 10722734.
- Schwer H, Liu LQ, Zhou L, Little MT, Pan Z, Hetherington CJ, Zhang DE (April 2000). "Cloning and characterization of a novel human ubiquitin-specific protease, a homologue of murine UBP43 (Usp18)". Genomics. 65 (1): 44–52. doi:10.1006/geno.2000.6148. PMID 10777664.
- Kang D, Jiang H, Wu Q, Pestka S, Fisher PB (April 2001). "Cloning and characterization of human ubiquitin-processing protease-43 from terminally differentiated human melanoma cells using a rapid subtraction hybridization protocol RaSH". Gene. 267 (2): 233–42. doi:10.1016/S0378-1119(01)00384-5. PMID 11313150.
- Tokarz S, Berset C, La Rue J, Friedman K, Nakayama K, Nakayama K, et al. (November 2004). "The ISG15 isopeptidase UBP43 is regulated by proteolysis via the SCFSkp2 ubiquitin ligase". The Journal of Biological Chemistry. 279 (45): 46424–30. doi:10.1074/jbc.M403189200. PMID 15342634.
- Wiemann S, Arlt D, Huber W, Wellenreuther R, Schleeger S, Mehrle A, et al. (October 2004). "From ORFeome to biology: a functional genomics pipeline". Genome Research. 14 (10B): 2136–44. doi:10.1101/gr.2576704. PMC 528930. PMID 15489336.
- Yan M, Luo JK, Ritchie KJ, Sakai I, Takeuchi K, Ren R, Zhang DE (July 2007). "Ubp43 regulates BCR-ABL leukemogenesis via the type 1 interferon receptor signaling". Blood. 110 (1): 305–12. doi:10.1182/blood-2006-07-033209. PMC 1896118. PMID 17374743.
- Ketscher L, Hannß R, Morales DJ, Basters A, Guerra S, Goldmann T, et al. (February 2015). "Selective inactivation of USP18 isopeptidase activity in vivo enhances ISG15 conjugation and viral resistance" (PDF). Proceedings of the National Academy of Sciences of the United States of America. 112 (5): 1577–82. Bibcode:2015PNAS..112.1577K. doi:10.1073/pnas.1412881112. PMC 4321242. PMID 25605921.