Microbiota are the range of microorganisms that may be commensal, mutualistic, or pathogenic found in and on all multicellular organisms, including plants. Microbiota include bacteria, archaea, protists, fungi, and viruses,[2][3] and have been found to be crucial for immunologic, hormonal, and metabolic homeostasis of their host.
The term microbiome describes either the collective genomes of the microbes that reside in an ecological niche or else the microbes themselves.[4][5][6]
The microbiome and host emerged during evolution as a synergistic unit from epigenetics and genetic characteristics, sometimes collectively referred to as a holobiont.[7][8] The presence of microbiota in human and other metazoan guts has been critical for understanding the co-evolution between metazoans and bacteria.[9][10] Microbiota play key roles in the intestinal immune and metabolic responses via their fermentation product (short-chain fatty acid), acetate.[11]
Introduction
editAll plants and animals, from simple life forms to humans, live in close association with microbial organisms.[12] Several advances have driven the perception of microbiomes, including:
- the ability to perform genomic and gene expression analyses of single cells and of entire microbial communities in the disciplines of metagenomics and metatranscriptomics[13]
- databases accessible to researchers across multiple disciplines[13]
- methods of mathematical analysis suitable for complex data sets[13]
Biologists have come to appreciate that microbes make up an important part of an organism's phenotype, far beyond the occasional symbiotic case study.[13]
Types of microbe-host relationships
editCommensalism, a concept developed by Pierre-Joseph van Beneden (1809–1894), a Belgian professor at the University of Louvain during the nineteenth century[14] is central to the microbiome, where microbiota colonize a host in a non-harmful coexistence. The relationship with their host is called mutualistic when organisms perform tasks that are known to be useful for the host,[15]: 700 [16] parasitic, when disadvantageous to the host. Other authors define a situation as mutualistic where both benefit, and commensal, where the unaffected host benefits the symbiont.[17] A nutrient exchange may be bidirectional or unidirectional, may be context dependent and may occur in diverse ways.[17] Microbiota that are expected to be present, and that under normal circumstances do not cause disease, are deemed normal flora or normal microbiota;[15] normal flora can not only be harmless, but can be protective of the host.[18]
Acquisition and change
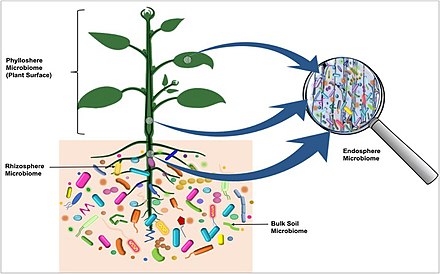
editThe initial acquisition of microbiota in animals from mammalians to marine sponges is at birth, and may even occur through the germ cell line. In plants, the colonizing process can be initiated below ground in the root zone, around the germinating seed, the spermosphere, or originate from the above ground parts, the phyllosphere and the flower zone or anthosphere.[19] The stability of the rhizosphere microbiota over generations depends upon the plant type but even more on the soil composition, i.e. living and non living environment.[20] Clinically, new microbiota can be acquired through fecal microbiota transplant to treat infections such as chronic C. difficile infection.[21]
Microbiota by host
editHumans
editThe human microbiota includes bacteria, fungi, archaea and viruses. Micro-animals which live on the human body are excluded. The human microbiome refers to their collective genomes.[15]
Humans are colonized by many microorganisms; the traditional estimate was that humans live with ten times more non-human cells than human cells; more recent estimates have lowered this to 3:1 and even to about 1:1 by number (1:350 by mass).[22][23][24][25][26]
In fact, these are so small that there are around 100 trillion microbiota on the human body,[27] around 39 trillion by revised estimates, with only 0.2 kg of total mass in a "reference" 70 kg human body.[26]
The Human Microbiome Project sequenced the genome of the human microbiota, focusing particularly on the microbiota that normally inhabit the skin, mouth, nose, digestive tract, and vagina.[15] It reached a milestone in 2012 when it published initial results.[28]
Non-human animals
edit- Amphibians have microbiota on their skin.[29] Some species are able to carry a fungus named Batrachochytrium dendrobatidis, which in others can cause a deadly infection Chytridiomycosis depending on their microbiome, resisting pathogen colonization or inhibiting their growth with antimicrobial skin peptides.[30]
- Newborn marsupials are born with histologically immature immune tissues and unable to mount their own specific immune defence. They are therefore heavily reliant on their mother's immune system[31] and the milk[32] for their protection. Most marsupials have pouches, and their own microbiota changes throughout the reproductive stages: oestrus, birth/oestrus, and post-oestrus.[33] Some pouch and skin secretions have had antimicrobial peptides identified, that presumably support the young at this vulnerable time.
- In mammals, herbivores such as cattle depend on their rumen microbiome to convert cellulose into proteins, short chain fatty acids, and gases. Culture methods cannot provide information on all microorganisms present. Comparative metagenomic studies yielded the surprising result that individual cattle possess markedly different community structures, predicted phenotype, and metabolic potentials,[34] even though they were fed identical diets, were housed together, and were apparently functionally identical in their utilization of plant cell wall resources.
- Mice have become the most studied mammalian regarding their microbiomes. The gut microbiota have been studied in relation to allergic airway disease, obesity, gastrointestinal diseases and diabetes. Perinatal shifting of microbiota through low dose antibiotics can have long-lasting effects on future susceptibility to allergic airway disease. The frequency of certain subsets of microbes has been linked to disease severity. The presence of specific microbes early in postnatal life, instruct future immune responses.[35][36] In gnotobiotic mice certain gut bacteria were found to transmit a particular phenotype to recipient germ-free mice, that promoted accumulation of colonic regulatory T cells, and strains that modulated mouse adiposity and cecal metabolite concentrations.[37] This combinatorial approach enables a systems-level understanding of microbial contributions to human biology.[38] But also other mucoide tissues as lung and vagina have been studied in relation to diseases such as asthma, allergy and vaginosis.[39]
- Insects have their own microbiomes. For example, leaf-cutter ants form huge underground colonies harvesting hundreds of kilograms of leaves each year and are unable to digest the cellulose in the leaves directly. They maintain fungus gardens as the colony's primary food source. While the fungus itself does not digest cellulose, a microbial community containing a diversity of bacteria is doing so. Analysis of the microbial population's genome revealed many genes with a role in cellulose digestion. This microbiome's predicted carbohydrate-degrading enzyme profile is similar to that of the bovine rumen, but the species composition is almost entirely different.[40] Gut microbiota of the fruit fly can affect the way its gut looks, by impacting epithelial renewal rate, cellular spacing, and the composition of different cell types in the epithelium.[41] When the moth Spodoptera exigua is infected with baculovirus immune-related genes are downregulated and the amount of its gut microbiota increases.[42] In the dipteran intestine, enteroendocrine cells sense the gut microbiota-derived metabolites and coordinate antibacterial, mechanical, and metabolic branches of the host intestinal innate immune response to the commensal microbiota.[43]
- Fish have their own microbiomes, including the short-lived species Nothobranchius furzeri (turquoise killifish). Transferring the gut microbiota from young killfish into middle-aged killifish significantly extends the lifespans of the middle-aged killfish.[44]
Plants
editThe plant microbiome was recently discovered to originate from the seed.[46] Microorganism which are transmitted via seed migrate into the developing seedling in a specific route in which certain community move to the leaves and others to the roots.[46] In the diagram on the right, microbiota colonizing the rhizosphere, entering the roots and colonizing the next tuber generation via the stolons, are visualized with a red color. Bacteria present in the mother tuber, passing through the stolons and migrating into the plant as well as into the next generation of tubers are shown in blue.[45]
- The soil is the main reservoir for bacteria that colonize potato tubers
- Bacteria are recruited from the soil more or less independent of the potato variety
- Bacteria might colonize the tubers predominantly from the inside of plants via the stolon
- The bacterial microbiota of potato tubers consists of bacteria transmitted from one tuber generation to the next and bacteria recruited from the soil colonize potato plants via the root.[45]
Plants are attractive hosts for microorganisms since they provide a variety of nutrients. Microorganisms on plants can be epiphytes (found on the plants) or endophytes (found inside plant tissue).[47][48] Oomycetes and fungi have, through convergent evolution, developed similar morphology and occupy similar ecological niches. They develop hyphae, threadlike structures that penetrate the host cell. In mutualistic situations the plant often exchanges hexose sugars for inorganic phosphate from the fungal symbiont. It is speculated that such very ancient associations have aided plants when they first colonized land.[17][49] Plant-growth promoting bacteria (PGPB) provide the plant with essential services such as nitrogen fixation, solubilization of minerals such as phosphorus, synthesis of plant hormones, direct enhancement of mineral uptake, and protection from pathogens.[50][51] PGPBs may protect plants from pathogens by competing with the pathogen for an ecological niche or a substrate, producing inhibitory allelochemicals, or inducing systemic resistance in host plants to the pathogen[19]
Research
editThe symbiotic relationship between a host and its microbiota is under laboratory research for how it may shape the immune system of mammals.[52][53] In many animals, the immune system and microbiota may engage in "cross-talk" by exchanging chemical signals, which may enable the microbiota to influence immune reactivity and targeting.[54] Bacteria can be transferred from mother to child through direct contact and after birth.[55] As the infant microbiome is established, commensal bacteria quickly populate the gut, prompting a range of immune responses and "programming" the immune system with long-lasting effects.[54] The bacteria are able to stimulate lymphoid tissue associated with the gut mucosa, which enables the tissue to produce antibodies for pathogens that may enter the gut.[54]
The human microbiome may play a role in the activation of toll-like receptors in the intestines, a type of pattern recognition receptor host cells use to recognize dangers and repair damage. Pathogens can influence this coexistence leading to immune dysregulation including and susceptibility to diseases, mechanisms of inflammation, immune tolerance, and autoimmune diseases.[56][57]
Co-evolution of microbiota
editOrganisms evolve within ecosystems so that the change of one organism affects the change of others. The hologenome theory of evolution proposes that an object of natural selection is not the individual organism, but the organism together with its associated organisms, including its microbial communities.
Coral reefs. The hologenome theory originated in studies on coral reefs.[58] Coral reefs are the largest structures created by living organisms, and contain abundant and highly complex microbial communities. Over the past several decades, major declines in coral populations have occurred. Climate change, water pollution and over-fishing are three stress factors that have been described as leading to disease susceptibility. Over twenty different coral diseases have been described, but of these, only a handful have had their causative agents isolated and characterized. Coral bleaching is the most serious of these diseases. In the Mediterranean Sea, the bleaching of Oculina patagonica was first described in 1994 and shortly determined to be due to infection by Vibrio shiloi. From 1994 to 2002, bacterial bleaching of O. patagonica occurred every summer in the eastern Mediterranean. Surprisingly, however, after 2003, O. patagonica in the eastern Mediterranean has been resistant to V. shiloi infection, although other diseases still cause bleaching. The surprise stems from the knowledge that corals are long lived, with lifespans on the order of decades,[59] and do not have adaptive immune systems.[citation needed] Their innate immune systems do not produce antibodies, and they should seemingly not be able to respond to new challenges except over evolutionary time scales.[citation needed]
The puzzle of how corals managed to acquire resistance to a specific pathogen led to a 2007 proposal, that a dynamic relationship exists between corals and their symbiotic microbial communities. It is thought that by altering its composition, the holobiont can adapt to changing environmental conditions far more rapidly than by genetic mutation and selection alone. Extrapolating this hypothesis to other organisms, including higher plants and animals, led to the proposal of the hologenome theory of evolution.[58]
As of 2007[update] the hologenome theory was still being debated.[60] A major criticism has been the claim that V. shiloi was misidentified as the causative agent of coral bleaching, and that its presence in bleached O. patagonica was simply that of opportunistic colonization.[61] If this is true, the basic observation leading to the theory would be invalid. The theory has gained significant popularity as a way of explaining rapid changes in adaptation that cannot otherwise be explained by traditional mechanisms of natural selection. Within the hologenome theory, the holobiont has not only become the principal unit of natural selection but also the result of other step of integration that it is also observed at the cell (symbiogenesis, endosymbiosis) and genomic levels.[7]
Research methods
editTargeted amplicon sequencing
editTargeted amplicon sequencing relies on having some expectations about the composition of the community that is being studied. In target amplicon sequencing a phylogenetically informative marker is targeted for sequencing. Such a marker should be present in ideally all the expected organisms. It should also evolve in such a way that it is conserved enough that primers can target genes from a wide range of organisms while evolving quickly enough to allow for finer resolution at the taxonomic level. A common marker for human microbiome studies is the gene for bacterial 16S rRNA (i.e. "16S rDNA", the sequence of DNA which encodes the ribosomal RNA molecule).[62] Since ribosomes are present in all living organisms, using 16S rDNA allows for DNA to be amplified from many more organisms than if another marker were used. The 16S rRNA gene contains both slowly evolving regions and 9 fast evolving regions, also known as hypervariable regions (HVRs);[63] the former can be used to design broad primers while the latter allow for finer taxonomic distinction. However, species-level resolution is not typically possible using the 16S rDNA. Primer selection is an important step, as anything that cannot be targeted by the primer will not be amplified and thus will not be detected, moreover different sets of primers can be selected to amplify different HVRs in the gene, or pairs of them. The appropriate choice of which HVRs to amplify has to be made according to the taxonomic groups of interest, as different target regions has been shown to influence taxonomical classification.[64]
Targeted studies of eukaryotic and viral communities are limited[65] and subject to the challenge of excluding host DNA from amplification and the reduced eukaryotic and viral biomass in the human microbiome.[66]
After the amplicons are sequenced, molecular phylogenetic methods are used to infer the composition of the microbial community. This can be done through clustering methodologies, by clustering the amplicons into operational taxonomic units (OTUs); or alternatively with denoising methodologies, identifying amplicon sequence variants (ASVs).
Phylogenetic relationships are then inferred between the sequences. Due to the complexity of the data, distance measures such as UniFrac distances are usually defined between microbiome samples, and downstream multivariate methods are carried out on the distance matrices. An important point is that the scale of data is extensive, and further approaches must be taken to identify patterns from the available information. Tools used to analyze the data include VAMPS,[67] QIIME,[68] mothur[69] and DADA2[70] or UNOISE3[71] for denoising.
Metagenomic sequencing
editMetagenomics is also used extensively for studying microbial communities.[72][73][74] In metagenomic sequencing, DNA is recovered directly from environmental samples in an untargeted manner with the goal of obtaining an unbiased sample from all genes of all members of the community. Recent studies use shotgun Sanger sequencing or pyrosequencing to recover the sequences of the reads.[75] The reads can then be assembled into contigs. To determine the phylogenetic identity of a sequence, it is compared to available full genome sequences using methods such as BLAST. One drawback of this approach is that many members of microbial communities do not have a representative sequenced genome, but this applies to 16S rRNA amplicon sequencing as well and is a fundamental problem.[62] With shotgun sequencing, it can be resolved by having a high coverage (50-100x) of the unknown genome, effectively doing a de novo genome assembly. As soon as there is a complete genome of an unknown organism available it can be compared phylogenetically and the organism put into its place in the tree of life, by creating new taxa. An emerging approach is to combine shotgun sequencing with proximity-ligation data (Hi-C) to assemble complete microbial genomes without culturing.[76]
Despite the fact that metagenomics is limited by the availability of reference sequences, one significant advantage of metagenomics over targeted amplicon sequencing is that metagenomics data can elucidate the functional potential of the community DNA.[77][78] Targeted gene surveys cannot do this as they only reveal the phylogenetic relationship between the same gene from different organisms. Functional analysis is done by comparing the recovered sequences to databases of metagenomic annotations such as KEGG. The metabolic pathways that these genes are involved in can then be predicted with tools such as MG-RAST,[79] CAMERA[80] and IMG/M.[81]
RNA and protein-based approaches
editMetatranscriptomics studies have been performed to study the gene expression of microbial communities through methods such as the pyrosequencing of extracted RNA.[82] Structure based studies have also identified non-coding RNAs (ncRNAs) such as ribozymes from microbiota.[83] Metaproteomics is an approach that studies the proteins expressed by microbiota, giving insight into its functional potential.[84]
Projects
editThe Human Microbiome Project launched in 2008 was a United States National Institutes of Health initiative to identify and characterize microorganisms found in both healthy and diseased humans.[85] The five-year project, best characterized as a feasibility study with a budget of $115 million, tested how changes in the human microbiome are associated with human health or disease.[85]
The Earth Microbiome Project (EMP) is an initiative to collect natural samples and analyze the microbial community around the globe. Microbes are highly abundant, diverse and have an important role in the ecological system. Yet as of 2010[update], it was estimated that the total global environmental DNA sequencing effort had produced less than 1 percent of the total DNA found in a liter of seawater or a gram of soil,[86] and the specific interactions between microbes are largely unknown. The EMP aims to process as many as 200,000 samples in different biomes, generating a complete database of microbes on earth to characterize environments and ecosystems by microbial composition and interaction. Using these data, new ecological and evolutionary theories can be proposed and tested.[87]
Gut microbiota and type 2 diabetes
editThe gut microbiota are very important for the host health because they play role in degradation of non-digestible polysaccharides (fermentation of resistant starch, oligosaccharides, inulin) strengthening gut integrity or shaping the intestinal epithelium, harvesting energy, protecting against pathogens, and regulating host immunity.[88][89]
Several studies showed that the gut bacterial composition in diabetic patients became altered with increased levels of Lactobacillus gasseri, Streptococcus mutans and Clostridiales members, with decrease in butyrate-producing bacteria such as Roseburia intestinalis and Faecalibacterium prausnitzii.[90][91] This alteration is due to many factors such as antibiotic abuse, diet, and age.
The decrease in butyrate production is associated with defects in intestinal permeability, which could lead to endotoxemia, which is the increased level of circulating Lipopolysaccharides from gram negative bacterial cells wall. It is found that endotoxemia has association with development of insulin resistance.[90]
In addition that butyrate production affects serotonin level.[90] Elevated serotonin level has contribution in obesity, which is known to be a risk factor for development of diabetes.
Gut microbiota development and antibiotics
editThe colonization of the human gut microbiota may start already before birth.[92] There are multiple factors in the environment that affects the development of the microbiota with birthmode being one of the most impactful.[93]
Another factor that has been observed to cause huge changes in the gut microbiota, particularly in children, is the use of antibiotics, associating with health issues such as higher BMI,[94][95] and further an increased risk towards metabolic diseases such as obesity.[96] In infants it was observed that amoxicillin and macrolides cause significant shifts in the gut microbiota characterized by a change in the bacterial classes Bifidobacteria, Enterobacteria and Clostridia.[97] A single course of antibiotics in adults causes changes in both the bacterial and fungal microbiota, with even more persistent changes in the fungal communities.[98] The bacteria and fungi live together in the gut and there is most likely a competition for nutrient sources present.[99][100] Seelbinder et al. found that commensal bacteria in the gut regulate the growth and pathogenicity of Candida albicans by their metabolites, particularly by propionate, acetic acid and 5-dodecenoate.[98] Candida has previously been associated with IBD[101] and further it has been observed to be increased in non-responders to a biological drug, infliximab, given to IBD patients with severe IBD.[102] Propionate and acetic acid are both short-chain fatty acids (SCFAs) that have been observed to be beneficial to gut microbiota health.[103][104][105] When antibiotics affect the growth of bacteria in the gut, there might be an overgrowth of certain fungi, which might be pathogenic when not regulated.[98]
Privacy issues
editMicrobial DNA inhabiting a person's human body can uniquely identify the person. A person's privacy may be compromised if the person anonymously donated microbe DNA data. Their medical condition and identity could be revealed.[106][107][108]
See also
editReferences
edit- ^ Dastogeer, K.M., Tumpa, F.H., Sultana, A., Akter, M.A. and Chakraborty, A. (2020) "Plant microbiome–an account of the factors that shape community composition and diversity". Current Plant Biology, 23: 100161. doi:10.1016/j.cpb.2020.100161. Material was copied from this source, which is available under a Creative Commons Attribution 4.0 International License.
- ^ De Sordi, Luisa; Lourenço, Marta; Debarbieux, Laurent (2019). "The battle within: interactions of bacteriophages and bacteria in the gastrointestinal tract". Cell Host & Microbe. 25 (2): 210–218. doi:10.1016/j.chom.2019.01.018. PMID 30763535. S2CID 73455329.
- ^ Peterson, J; Garges, S; et al. (2009). "The NIH Human Microbiome Project". Genome Research. 19 (12). NIH HMP Working Group: 2317–2323. doi:10.1101/gr.096651.109. PMC 2792171. PMID 19819907.
- ^ Backhed, F.; Ley, R. E.; Sonnenburg, J. L.; Peterson, D. A.; Gordon, J. I. (2005). "Host-Bacterial Mutualism in the Human Intestine". Science. 307 (5717): 1915–1920. Bibcode:2005Sci...307.1915B. doi:10.1126/science.1104816. PMID 15790844. S2CID 6332272.
- ^ Turnbaugh, P. J.; Ley, R. E.; Hamady, M.; Fraser-Liggett, C. M.; Knight, R.; Gordon, J. I. (2007). "The Human Microbiome Project". Nature. 449 (7164): 804–810. Bibcode:2007Natur.449..804T. doi:10.1038/nature06244. PMC 3709439. PMID 17943116.
- ^ Ley, R. E.; Peterson, D. A.; Gordon, J. I. (2006). "Ecological and Evolutionary Forces Shaping Microbial Diversity in the Human Intestine". Cell. 124 (4): 837–848. doi:10.1016/j.cell.2006.02.017. PMID 16497592. S2CID 17203181.
- ^ a b Salvucci, E. (2016). "Microbiome, holobiont and the net of life". Critical Reviews in Microbiology. 42 (3): 485–494. doi:10.3109/1040841X.2014.962478. hdl:11336/33456. PMID 25430522. S2CID 30677140.
- ^ Guerrero, R.; Margulis, Lynn; Berlanga, M. (2013). "Symbiogenesis: The holobiont as a unit of evolution". International Microbiology. 16 (3): 133–143. doi:10.2436/20.1501.01.188. PMID 24568029.
- ^ Davenport, Emily R et al. "The human microbiome in evolution". BMC Biology. vol. 15,1 127. 27 Dec. 2017, doi:10.1186/s12915-017-0454-7
- ^ "Evolution of the human gut flora". Andrew H. Moeller, Yingying Li, Eitel Mpoudi Ngole, Steve Ahuka-Mundeke, Elizabeth V. Lonsdorf, Anne E. Pusey, Martine Peeters, Beatrice H. Hahn, Howard Ochman. Proceedings of the National Academy of Sciences. Nov 2014, 111 (46) 16431–16435; doi:10.1073/pnas.1419136111
- ^ Jugder, Bat-Erdene; Kamareddine, Layla; Watnick, Paula I. (2021). "Microbiota-derived acetate activates intestinal innate immunity via the Tip60 histone acetyltransferase complex". Immunity. 54 (8): 1683–1697.e3. doi:10.1016/j.immuni.2021.05.017. ISSN 1074-7613. PMC 8363570. PMID 34107298.
- ^ Mendes, R.; Raaijmakers, J.M. (2015). "Cross-kingdom similarities in microbiome functions". The ISME Journal. 9 (9): 1905–1907. Bibcode:2015ISMEJ...9.1905M. doi:10.1038/ismej.2015.7. PMC 4542044. PMID 25647346.
- ^ a b c d Bosch, T. C. G.; McFall-Ngai, M. J. (2011). "Metaorganisms as the new frontier". Zoology. 114 (4): 185–190. Bibcode:2011Zool..114..185B. doi:10.1016/j.zool.2011.04.001. PMC 3992624. PMID 21737250.
- ^ Poreau B., Biologie et complexité : histoire et modèles du commensalisme. PhD Dissertation, University of Lyon, France, 2014.
- ^ a b c d Sherwood, Linda; Willey, Joanne; Woolverton, Christopher (2013). Prescott's Microbiology (9th ed.). New York: McGraw Hill. pp. 713–721. ISBN 9780073402406. OCLC 886600661.
- ^ Quigley, E. M. (Sep 2013). "Gut bacteria in health and disease". Gastroenterol Hepatol (N Y). 9 (9): 560–569. PMC 3983973. PMID 24729765.
- ^ a b c Remy W, Taylor TN, Hass H, Kerp H (1994). "Four hundred-million-year-old vesicular arbuscular mycorrhizae". Proc. Natl. Acad. Sci. USA. 91 (25): 11841–11843. Bibcode:1994PNAS...9111841R. doi:10.1073/pnas.91.25.11841. PMC 45331. PMID 11607500.
- ^ Copeland, CS (Sep–Oct 2017). "The World Within Us". Healthcare Journal of New Orleans. Archived from the original on 2019-12-07. Retrieved 2019-12-07.
- ^ a b Compant S, Duffy B, Nowak J, Clément C, Barka EA (2005). "Use of Plant Growth-Promoting Bacteria for Biocontrol of Plant Diseases: Principles, Mechanisms of Action, and Future Prospects". Appl Environ Microbiol. 71 (9): 4951–4959. Bibcode:2005ApEnM..71.4951C. doi:10.1128/AEM.71.9.4951-4959.2005. PMC 1214602. PMID 16151072.
- ^ Tkacz, Andrzej; Cheema, Jitender; Chandra, Govind; Grant, Alastair; Poole, Philip S. (Nov 2015). "Stability and succession of the rhizosphere microbiota depends upon plant type and soil composition". ISME J. 9 (11): 2349–2359. Bibcode:2015ISMEJ...9.2349T. doi:10.1038/ismej.2015.41. PMC 4611498. PMID 25909975.
- ^ Copeland, CS (19 April 2019). "What is Clostridium difficile?". Vitalacy.
- ^ American Academy of Microbiology FAQ: Human Microbiome Archived 2016-12-31 at the Wayback Machine January 2014
- ^ Judah L. Rosner for Microbe Magazine, Feb 2014. Ten Times More Microbial Cells than Body Cells in Humans?
- ^ Alison Abbott for Nature News. Jan 8 2016 Scientists bust myth that our bodies have more bacteria than human cells
- ^ Sender, R; Fuchs, S; Milo, R (Jan 2016). "Are We Really Vastly Outnumbered? Revisiting the Ratio of Bacterial to Host Cells in Humans". Cell. 164 (3): 337–340. doi:10.1016/j.cell.2016.01.013. PMID 26824647. S2CID 1790146.
- ^ a b Sender, Ron; Fuchs, Shai; Milo, Ron (2016-08-19). "Revised Estimates for the Number of Human and Bacteria Cells in the Body". PLOS Biology. 14 (8): e1002533. doi:10.1371/journal.pbio.1002533. PMC 4991899. PMID 27541692.
- ^ "On and in You." Micropia, www.micropia.nl/en/discover/stories/on-and-in-you/#:~:text=They're%20on%20you%2C%20in,re%20known%20as%20human%20microbiota.
- ^ "NIH Human Microbiome Project defines normal bacterial makeup of the body". NIH News. 13 June 2012.
- ^ Bataille, A; Lee-Cruz, L; Tripathi, B; Kim, H; Waldman, B (Jan 2016). "Microbiome Variation Across Amphibian Skin Regions: Implications for Chytridiomycosis Mitigation Efforts". Microb. Ecol. 71 (1): 221–232. Bibcode:2016MicEc..71..221B. doi:10.1007/s00248-015-0653-0. PMID 26271741. S2CID 12951957.
- ^ Woodhams DC, Rollins-Smith LA, Alford RA, Simon MA, Harris RN (2007). "Innate immune defenses of amphibian skin: antimicrobial peptides and more". Animal Conservation. 10 (4): 425–428. Bibcode:2007AnCon..10..425W. doi:10.1111/j.1469-1795.2007.00150.x. S2CID 84293044.
- ^ Old JM, Deane EM (2000). "Development of the immune system and immunological protection in marsupial pouch young". Developmental and Comparative Immunology. 24 (5): 445–454. doi:10.1016/S0145-305X(00)00008-2. PMID 10785270.
- ^ Stannard HJ, Miller RD, Old JM (2020). "Marsupial and monotreme milk – a review of its nutrients and immune properties". PeerJ. 8: e9335. doi:10.7717/peerj.9335. PMC 7319036. PMID 32612884.
- ^ Old JM, Deane EM (1998). "The effect of oestrus and the presence of pouch young on aerobic bacteria isolated from the pouch of the tammar wallaby, Macropus eugenii". Comparative Immunology Microbiology and Infectious Diseases. 21 (4): 237–245. doi:10.1016/s0147-9571(98)00022-8. PMID 9775355.
- ^ Brulc JM; Antonopoulos DA; Miller MEB; et al. (2009). "Gene-centric metagenomics of the fiber-adherent bovine rumen microbiome reveals forage specific glycoside hydrolases". Proc. Natl. Acad. Sci. USA. 106 (6): 1948–1953. Bibcode:2009PNAS..106.1948B. doi:10.1073/pnas.0806191105. PMC 2633212. PMID 19181843.
- ^ Russell SL, Gold MJ; et al. (May 2012). "Early life antibiotic-driven changes in microbiota enhance susceptibility to allergic asthma". EMBO Rep. 13 (5): 440–447. doi:10.1038/embor.2012.32. PMC 3343350. PMID 22422004.
- ^ Russell SL, Gold MJ, et al. (Aug 2014). "Perinatal antibiotic-induced shifts in gut microbiota have differential effects on inflammatory lung diseases". J Allergy Clin Immunol. 135 (1): 100–109. doi:10.1016/j.jaci.2014.06.027. PMID 25145536.
- ^ Turnbaugh PJ, et al. (Dec 2006). "An obesity-associated gut microbiome with increased capacity for energy harvest". Nature. 444 (7122): 1027–1031. Bibcode:2006Natur.444.1027T. doi:10.1038/nature05414. PMID 17183312. S2CID 4400297.
- ^ Faith JJ, Ahern PP, Ridaura VK, et al. (Jan 2014). "Identifying gut microbe-host phenotype relationships using combinatorial communities in gnotobiotic mice". Sci. Transl. Med. 6 (220): 220. doi:10.1126/scitranslmed.3008051. PMC 3973144. PMID 24452263.
- ^ Barfod, KK; Roggenbuck, M; Hansen, LH; Schjørring, S; Larsen, ST; Sørensen, SJ; Krogfelt, KA (2013). "The murine lung microbiome in relation to the intestinal and vaginal bacterial communities". BMC Microbiol. 13: 303. doi:10.1186/1471-2180-13-303. PMC 3878784. PMID 24373613.
- ^ Suen; Scott JJ; Aylward FO; et al. (2010). Sonnenburg, Justin (ed.). "An Insect Herbivore Microbiome with High Plant Biomass-Degrading Capacity". PLOS Genet. 6 (9): e1001129. doi:10.1371/journal.pgen.1001129. PMC 2944797. PMID 20885794.
- ^ Broderick, Nichole A.; Buchon, Nicolas; Lemaitre, Bruno (2014). "Microbiota-Induced Changes in Drosophila melanogaster Host Gene Expression and Gut Morphology". mBio. 5 (3): e01117–14. doi:10.1128/mBio.01117-14. PMC 4045073. PMID 24865556.
- ^ Jakubowska, Agata K.; Vogel, Heiko; Herrero, Salvador (May 2013). "Increase in Gut Microbiota after Immune Suppression in Baculovirus-infected Larvae". PLOS Pathog. 9 (5): e1003379. doi:10.1371/journal.ppat.1003379. PMC 3662647. PMID 23717206.
- ^ Watnick, Paula I.; Jugder, Bat-Erdene (2020-02-01). "Microbial Control of Intestinal Homeostasis via Enteroendocrine Cell Innate Immune Signaling". Trends in Microbiology. 28 (2): 141–149. doi:10.1016/j.tim.2019.09.005. ISSN 0966-842X. PMC 6980660. PMID 31699645.
- ^ Tibbs TN, Lopez LR, Arthur JC (2019). "The influence of the microbiota on immune development, chronic inflammation, and cancer in the context of aging". Microbial Cell. 6 (8): 324–334. doi:10.15698/mic2019.08.685 (inactive 1 November 2024). PMC 6685047. PMID 31403049.
{{cite journal}}: CS1 maint: DOI inactive as of November 2024 (link) - ^ a b c Buchholz, F., Antonielli, L., Kostić, T., Sessitsch, A. and Mitter, B. (2019) "The bacterial community in potato is recruited from soil and partly inherited across generations". PLOS One, 14(11): e0223691. doi:10.1371/journal.pone.0223691. Material was copied from this source, which is available under a Creative Commons Attribution 4.0 International License.
- ^ a b Abdelfattah, Ahmed; Wisniewski, Michael; Schena, Leonardo; Tack, Ayco J. M. (2021). "Experimental evidence of microbial inheritance in plants and transmission routes from seed to phyllosphere and root". Environmental Microbiology. 23 (4): 2199–2214. Bibcode:2021EnvMi..23.2199A. doi:10.1111/1462-2920.15392. ISSN 1462-2920. PMID 33427409. S2CID 231576517.
- ^ Berlec, Aleš (2012-09-01). "Novel techniques and findings in the study of plant microbiota: Search for plant probiotics". Plant Science. 193–194: 96–102. Bibcode:2012PlnSc.193...96B. doi:10.1016/j.plantsci.2012.05.010. PMID 22794922.
- ^ Whipps, J.m.; Hand, P.; Pink, D.; Bending, G.d. (2008-12-01). "Phyllosphere microbiology with special reference to diversity and plant genotype" (PDF). Journal of Applied Microbiology. 105 (6): 1744–1755. doi:10.1111/j.1365-2672.2008.03906.x. ISSN 1365-2672. PMID 19120625. S2CID 35055151.
- ^ Chibucos MC, Tyler BM (2009). "Common themes in nutrient acquisition by plant symbiotic microbes, described by the Gene Ontology". BMC Microbiology. 9(Suppl 1) (Suppl 1): S6. doi:10.1186/1471-2180-9-S1-S6. PMC 2654666. PMID 19278554.
- ^ Kloepper, J. W (1993). "Plant growth-promoting rhizobacteria as biological control agents". In Metting, F. B. Jr (ed.). Soil microbial ecology: applications in agricultural and environmental management. New York: Marcel Dekker Inc. pp. 255–274. ISBN 978-0-8247-8737-0.
- ^ Bloemberg, G. V.; Lugtenberg, B. J. J. (2001). "Molecular basis of plant growth promotion and biocontrol by rhizobacteria". Current Opinion in Plant Biology. 4 (4): 343–350. Bibcode:2001COPB....4..343B. doi:10.1016/S1369-5266(00)00183-7. PMID 11418345.
- ^ Palm, Noah W.; de Zoete, Marcel R.; Flavell, Richard A. (30 June 2015). "Immune–microbiota interactions in health and disease". Clinical Immunology. 159 (2): 122–127. doi:10.1016/j.clim.2015.05.014. ISSN 1521-6616. PMC 4943041. PMID 26141651.
- ^ Round, June L.; O'Connell, Ryan M.; Mazmanian, Sarkis K. (2010). "Coordination of tolerogenic immune responses by the commensal microbiota". Journal of Autoimmunity. 34 (3): J220–J225. doi:10.1016/j.jaut.2009.11.007. PMC 3155383. PMID 19963349.
- ^ a b c Cahenzli, Julia; Balmer, Maria L.; McCoy, Kathy D. (2012). "Microbial-immune cross-talk and regulation of the immune system". Immunology. 138 (1): 12–22. doi:10.1111/j.1365-2567.2012.03624.x. PMC 3533697. PMID 22804726.
- ^ Rosenberg, Eugene; Zilber-Rosenberg, Ilana (2016). "Microbes drive evolution of animals and plants: the hologenome concept". mBio. 7 (2): e01395–15. doi:10.1128/mbio.01395-15. PMC 4817260. PMID 27034283.
- ^ Blander, J Magarian; Longman, Randy S; Iliev, Iliyan D; Sonnenberg, Gregory F; Artis, David (19 July 2017). "Regulation of inflammation by microbiota interactions with the host". Nature Immunology. 18 (8): 851–860. doi:10.1038/ni.3780. ISSN 1529-2908. PMC 5800875. PMID 28722709.
- ^ Nikoopour, E; Singh, B (2014). "Reciprocity in microbiome and immune system interactions and its implications in disease and health". Inflamm Allergy Drug Targets. 13 (2): 94–104. doi:10.2174/1871528113666140330201056. PMID 24678760.
- ^ a b Rosenberg E, Koren O, Reshef L, Efrony R, Zilber-Rosenberg I (2007). "The role of microorganisms in coral health, disease and evolution". Nature Reviews Microbiology. 5 (5): 355–362. doi:10.1038/nrmicro1635. PMID 17384666. S2CID 2967190.
- ^ Baird AH, Bhagooli R, Ralph PJ, Takahashi S (2009). "Coral bleaching: the role of the host" (PDF). Trends in Ecology and Evolution. 24 (1): 16–20. Bibcode:2009TEcoE..24...16B. doi:10.1016/j.tree.2008.09.005. PMID 19022522.
- ^ Leggat W, Ainsworth T, Bythell J, Dove S, Gates R, Hoegh-Guldberg O, Iglesias-Prieto R, Yellowlees D (2007). "The hologenome theory disregards the coral holobiont". Nature Reviews Microbiology. 5 (10): Online Correspondence. doi:10.1038/nrmicro1635-c1. S2CID 9031305.
- ^ Ainsworth TD, Fine M, Roff G, Hoegh-Guldberg O (2008). "Bacteria are not the primary cause of bleaching in the Mediterranean coral Oculina patagonica". The ISME Journal. 2 (1): 67–73. Bibcode:2008ISMEJ...2...67A. doi:10.1038/ismej.2007.88. PMID 18059488. S2CID 1032896.
- ^ a b Kuczynski, J.; Lauber, C. L.; Walters, W. A.; Parfrey, L. W.; Clemente, J. C.; Gevers, D.; Knight, R. (2011). "Experimental and analytical tools for studying the human microbiome". Nature Reviews Genetics. 13 (1): 47–58. doi:10.1038/nrg3129. PMC 5119550. PMID 22179717.
- ^ Chakravorty, Soumitesh; Helb, Danica; Burday, Michele; Connell, Nancy; Alland, David (May 2007). "A detailed analysis of 16S ribosomal RNA gene segments for the diagnosis of pathogenic bacteria". Journal of Microbiological Methods. 69 (2): 330–339. doi:10.1016/j.mimet.2007.02.005. PMC 2562909. PMID 17391789.
- ^ Soriano-Lerma, Ana; Pérez-Carrasco, Virginia; Sánchez-Marañón, Manuel; Ortiz-González, Matilde; Sánchez-Martín, Victoria; Gijón, Juan; Navarro-Mari, José María; García-Salcedo, José Antonio; Soriano, Miguel (December 2020). "Influence of 16S rRNA target region on the outcome of microbiome studies in soil and saliva samples". Scientific Reports. 10 (1): 13637. Bibcode:2020NatSR..1013637S. doi:10.1038/s41598-020-70141-8. ISSN 2045-2322. PMC 7423937. PMID 32788589.
- ^ Marchesi, J. R. (2010). "Prokaryotic and Eukaryotic Diversity of the Human Gut". Advances in Applied Microbiology Volume 72. Vol. 72. pp. 43–62. doi:10.1016/S0065-2164(10)72002-5. ISBN 9780123809896. PMID 20602987.
- ^ Vestheim, H.; Jarman, S. N. (2008). "Blocking primers to enhance PCR amplification of rare sequences in mixed samples – a case study on prey DNA in Antarctic krill stomachs". Frontiers in Zoology. 5: 12. doi:10.1186/1742-9994-5-12. PMC 2517594. PMID 18638418.
- ^ "VAMPS: The Visualization and Analysis of Microbial Population Structures". Bay Paul Center, MBL, Woods Hole. Retrieved 11 March 2012.
- ^ Caporaso, J. G.; Kuczynski, J.; Stombaugh, J.; Bittinger, K.; Bushman, F. D.; Costello, E. K.; Fierer, N.; Peña, A. G.; Goodrich, J. K.; Gordon, J. I.; Huttley, G. A.; Kelley, S. T.; Knights, D.; Koenig, J. E.; Ley, R. E.; Lozupone, C. A.; McDonald, D.; Muegge, B. D.; Pirrung, M.; Reeder, J.; Sevinsky, J. R.; Turnbaugh, P. J.; Walters, W. A.; Widmann, J.; Yatsunenko, T.; Zaneveld, J.; Knight, R. (2010). "QIIME allows analysis of high-throughput community sequencing data". Nature Methods. 7 (5): 335–336. doi:10.1038/nmeth.f.303. PMC 3156573. PMID 20383131.
- ^ Schloss, P. D.; Westcott, S. L.; Ryabin, T.; Hall, J. R.; Hartmann, M.; Hollister, E. B.; Lesniewski, R. A.; Oakley, B. B.; Parks, D. H.; Robinson, C. J.; Sahl, J. W.; Stres, B.; Thallinger, G. G.; Van Horn, D. J.; Weber, C. F. (2009). "Introducing mothur: Open-Source, Platform-Independent, Community-Supported Software for Describing and Comparing Microbial Communities". Applied and Environmental Microbiology. 75 (23): 7537–7541. Bibcode:2009ApEnM..75.7537S. doi:10.1128/AEM.01541-09. PMC 2786419. PMID 19801464.
- ^ Callahan, Benjamin J.; McMurdie, Paul J.; Rosen, Michael J.; Han, Andrew W.; Johnson, Amy Jo A.; Holmes, Susan P. (July 2016). "DADA2: High-resolution sample inference from Illumina amplicon data". Nature Methods. 13 (7): 581–583. doi:10.1038/nmeth.3869. ISSN 1548-7105. PMC 4927377. PMID 27214047.
- ^ Edgar, Robert C. (2016-10-15). "UNOISE2: improved error-correction for Illumina 16S and ITS amplicon sequencing": 081257. doi:10.1101/081257. S2CID 784388.
{{cite journal}}: Cite journal requires|journal=(help) - ^ Turnbaugh, P. J.; Hamady, M.; Yatsunenko, T.; Cantarel, B. L.; Duncan, A.; Ley, R. E.; Sogin, M. L.; Jones, W. J.; Roe, B. A.; Affourtit, J. P.; Egholm, M.; Henrissat, B.; Heath, A. C.; Knight, R.; Gordon, J. I. (2008). "A core gut microbiome in obese and lean twins". Nature. 457 (7228): 480–484. Bibcode:2009Natur.457..480T. doi:10.1038/nature07540. PMC 2677729. PMID 19043404.
- ^ Qin, J.; Li, R.; Raes, J.; Arumugam, M.; Burgdorf, K. S.; Manichanh, C.; Nielsen, T.; Pons, N.; Levenez, F.; Yamada, T.; Mende, D. R.; Li, J.; Xu, J.; Li, S.; Li, D.; Cao, J.; Wang, B.; Liang, H.; Zheng, H.; Xie, Y.; Tap, J.; Lepage, P.; Bertalan, M.; Batto, J. M.; Hansen, T.; Le Paslier, D.; Linneberg, A.; Nielsen, H. B. R.; Pelletier, E.; Renault, P. (2010). "A human gut microbial gene catalogue established by metagenomic sequencing". Nature. 464 (7285): 59–65. Bibcode:2010Natur.464...59.. doi:10.1038/nature08821. PMC 3779803. PMID 20203603.
- ^ Tringe, S. G.; Von Mering, C.; Kobayashi, A.; Salamov, A. A.; Chen, K.; Chang, H. W.; Podar, M.; Short, J. M.; Mathur, E. J.; Detter, J. C.; Bork, P.; Hugenholtz, P.; Rubin, E. M. (2005). "Comparative Metagenomics of Microbial Communities". Science. 308 (5721): 554–557. Bibcode:2005Sci...308..554T. CiteSeerX 10.1.1.377.2288. doi:10.1126/science.1107851. PMID 15845853. S2CID 161283.
- ^ Wooley, J. C.; Godzik, A.; Friedberg, I. (2010). Bourne, Philip E. (ed.). "A Primer on Metagenomics". PLOS Computational Biology. 6 (2): e1000667. Bibcode:2010PLSCB...6E0667W. doi:10.1371/journal.pcbi.1000667. PMC 2829047. PMID 20195499.
- ^ Watson, Mick; Roehe, Rainer; Walker, Alan W.; Dewhurst, Richard J.; Snelling, Timothy J.; Ivan Liachko; Langford, Kyle W.; Press, Maximilian O.; Wiser, Andrew H. (2018-02-28). "Assembly of 913 microbial genomes from metagenomic sequencing of the cow rumen". Nature Communications. 9 (1): 870. Bibcode:2018NatCo...9..870S. doi:10.1038/s41467-018-03317-6. ISSN 2041-1723. PMC 5830445. PMID 29491419.
- ^ Muller, J.; Szklarczyk, D.; Julien, P.; Letunic, I.; Roth, A.; Kuhn, M.; Powell, S.; Von Mering, C.; Doerks, T.; Jensen, L. J.; Bork, P. (2009). "EggNOG v2.0: Extending the evolutionary genealogy of genes with enhanced non-supervised orthologous groups, species and functional annotations". Nucleic Acids Research. 38 (Database issue): D190–D195. doi:10.1093/nar/gkp951. PMC 2808932. PMID 19900971.
- ^ Kanehisa, M.; Goto, S.; Furumichi, M.; Tanabe, M.; Hirakawa, M. (2009). "KEGG for representation and analysis of molecular networks involving diseases and drugs". Nucleic Acids Research. 38 (Database issue): D355–D360. doi:10.1093/nar/gkp896. PMC 2808910. PMID 19880382.
- ^ Meyer, F.; Paarmann, D.; d'Souza, M.; Olson, R.; Glass, E. M.; Kubal, M.; Paczian, T.; Rodriguez, A.; Stevens, R.; Wilke, A.; Wilkening, J.; Edwards, R. A. (2008). "The metagenomics RAST server – a public resource for the automatic phylogenetic and functional analysis of metagenomes". BMC Bioinformatics. 9: 386. doi:10.1186/1471-2105-9-386. PMC 2563014. PMID 18803844.
- ^ Sun, S.; Chen, J.; Li, W.; Altintas, I.; Lin, A.; Peltier, S.; Stocks, K.; Allen, E. E.; Ellisman, M.; Grethe, J.; Wooley, J. (2010). "Community cyberinfrastructure for Advanced Microbial Ecology Research and Analysis: The CAMERA resource". Nucleic Acids Research. 39 (Database issue): D546–D551. doi:10.1093/nar/gkq1102. PMC 3013694. PMID 21045053.
- ^ Markowitz, V. M.; Ivanova, N. N.; Szeto, E.; Palaniappan, K.; Chu, K.; Dalevi, D.; Chen, I. M. A.; Grechkin, Y.; Dubchak, I.; Anderson, I.; Lykidis, A.; Mavromatis, K.; Hugenholtz, P.; Kyrpides, N. C. (2007). "IMG/M: A data management and analysis system for metagenomes". Nucleic Acids Research. 36 (Database issue): D534–D538. doi:10.1093/nar/gkm869. PMC 2238950. PMID 17932063.
- ^ Shi, Y.; Tyson, G. W.; Delong, E. F. (2009). "Metatranscriptomics reveals unique microbial small RNAs in the ocean's water column". Nature. 459 (7244): 266–269. Bibcode:2009Natur.459..266S. doi:10.1038/nature08055. PMID 19444216. S2CID 4340144.
- ^ Jimenez, R. M.; Delwart, E.; Luptak, A (2011). "Structure-based Search Reveals Hammerhead Ribozymes in the Human Microbiome". Journal of Biological Chemistry. 286 (10): 7737–7743. doi:10.1074/jbc.C110.209288. PMC 3048661. PMID 21257745.
- ^ Maron, PA; Ranjard, L.; Mougel, C.; Lemanceau, P. (2007). "Metaproteomics: A New Approach for Studying Functional Microbial Ecology". Microbial Ecology. 53 (3): 486–493. Bibcode:2007MicEc..53..486M. doi:10.1007/s00248-006-9196-8. PMID 17431707. S2CID 26953155.
- ^ a b "NIH Human Microbiome Project". US National Institutes of Health, Department of Health and Human Services, US Government. 2016. Archived from the original on 11 June 2016. Retrieved 14 June 2016.
- ^ Gilbert, J. A.; Meyer, F.; Antonopoulos, D.; et al. (2010). "Meeting Report: The Terabase Metagenomics Workshop and the Vision of an Earth Microbiome Project". Standards in Genomic Sciences. 3 (3): 243–248. doi:10.4056/sigs.1433550. PMC 3035311. PMID 21304727.
- ^ Gilbert, J. A.; O'Dor, R.; King, N.; Vogel, T. M. (2011). "The importance of metagenomic surveys to microbial ecology: Or why Darwin would have been a metagenomic scientist". Microbial Informatics and Experimentation. 1 (1): 5. doi:10.1186/2042-5783-1-5. PMC 3348666. PMID 22587826.
- ^ Ibrahim, Nesma (2018-07-01). "Gut Microbiota and Type 2 Diabetes Mellitus : What is The Link ?". Afro-Egyptian Journal of Infectious and Endemic Diseases. 6 (2): 112–119. doi:10.21608/aeji.2018.9950. ISSN 2090-7184. S2CID 3900880.
- ^ Thursby, Elizabeth; Juge, Nathalie (2017-06-01). "Introduction to the human gut microbiota". Biochemical Journal. 474 (11): 1823–1836. doi:10.1042/BCJ20160510. ISSN 0264-6021. PMC 5433529. PMID 28512250.
- ^ a b c Muñoz-Garach, Araceli; Diaz-Perdigones, Cristina; Tinahones, Francisco J. (December 2016). "Microbiota y diabetes mellitus tipo 2". Endocrinología y Nutrición (in Spanish). 63 (10): 560–568. doi:10.1016/j.endonu.2016.07.008. PMID 27633134.
- ^ Blandino, G.; Inturri, R.; Lazzara, F.; Di Rosa, M.; Malaguarnera, L. (2016-11-01). "Impact of gut microbiota on diabetes mellitus". Diabetes & Metabolism. 42 (5): 303–315. doi:10.1016/j.diabet.2016.04.004. ISSN 1262-3636. PMID 27179626.
- ^ Vandenplas, Y., Carnielli, V. P., Ksiazyk, J., Luna, M. S., Migacheva, N., Mosselmans, J. M., ... & Wabitsch, M. (2020), Factors affecting early-life intestinal microbiota development. Nutrition, 78, 110812.
- ^ Korpela K, Helve O, Kolho KL, Saisto T, Skogberg K, Dikareva E, Stefanovic V, Salonen A, Andersson S, de Vos WM. Maternal Fecal Microbiota Transplantation in Cesarean-Born Infants Rapidly Restores Normal Gut Microbial Development: A Proof-of-Concept Study. Cell. 2020 Oct 15;183(2):324-334.e5. doi: 10.1016/j.cell.2020.08.047. Epub 2020 Oct 1. PMID 33007265.
- ^ Korpela, K., Salonen, A., Saxen, H., Nikkonen, A., Peltola, V., Jaakkola, T., ... & Kolho, K. L. (2020). Antibiotics in early life associate with specific gut microbiota signatures in a prospective longitudinal infant cohort. Pediatric Research, 1-6
- ^ Schei, K., Simpson, M. R., Avershina, E., Rudi, K., Øien, T., Júlíusson, P. B., ... & Ødegård, R. A. (2020). Early Gut Fungal and Bacterial Microbiota and Childhood Growth. Frontiers in pediatrics, 8, 658
- ^ Korpela, K., Salonen, A., Virta, L. J., Kekkonen, R. A., Forslund, K., Bork, P., & De Vos, W. M. (2016). Intestinal microbiome is related to lifetime antibiotic use in Finnish pre-school children. Nature communications, 7, 10410
- ^ Korpela, K., Salonen, A., Saxen, H., Nikkonen, A., Peltola, V., Jaakkola, T., ... & Kolho, K. L. (2020). Antibiotics in early life associate with specific gut microbiota signatures in a prospective longitudinal infant cohort. Pediatric Research, 1-6.
- ^ a b c Seelbinder, B., Chen, J., Brunke, S., Vazquez-Uribe, R., Santhaman, R., Meyer, A. C., ... & Panagiotou, G. (2020). Antibiotics create a shift from mutualism to competition in human gut communities with a longer-lasting impact on fungi than bacteria. Microbiome, 8(1), 1-20
- ^ Cabral, D. J., Penumutchu, S., Norris, C., Morones-Ramirez, J. R., & Belenky, P. (2018). Microbial competition between Escherichia coli and Candida albicans reveals a soluble fungicidal factor. Microbial cell, 5(5), 249
- ^ Peleg, A. Y., Hogan, D. A., & Mylonakis, E. (2010). Medically important bacterial–fungal interactions. Nature Reviews Microbiology, 8(5), 340-349
- ^ Sokol H, Leducq V, Aschard H, Pham H P, Jegou S, Landman C, Cohen D, Liguori G, Bourrier A, Nion-Larmurier I, Cosnes J, Seksik P, Langella P, Skurnik D, Richard ML, Beaugerie L. Fungal microbiota dysbiosis in IBD. Gut 2017;66:1039–1048. doi: 10.1136/gutjnl-2015-310746
- ^ Rebecka Ventin-Holmberg, Anja Eberl, Schahzad Saqib, Katri Korpela, Seppo Virtanen, Taina Sipponen, Anne Salonen, Päivi Saavalainen, Eija Nissilä, Bacterial and Fungal Profiles as Markers of Infliximab Drug Response in Inflammatory Bowel Disease, Journal of Crohn's and Colitis, 2020;, jjaa252, https://doi.org/10.1093/ecco-jcc/jjaa252
- ^ El Hage, R., Hernandez-Sanabria, E., Calatayud Arroyo, M., Props, R., & Van de Wiele, T. (2019). Propionate-producing consortium restores antibiotic-induced dysbiosis in a dynamic in vitro model of the human intestinal microbial ecosystem. Frontiers in microbiology, 10, 1206.
- ^ Tian, X., Hellman, J., Horswill, A. R., Crosby, H. A., Francis, K. P., & Prakash, A. (2019). Elevated gut microbiome-derived propionate levels are associated with reduced sterile lung inflammation and bacterial immunity in mice. Frontiers in microbiology, 10, 159.
- ^ Li, Y., Faden, H. S., & Zhu, L. (2020). The response of the gut microbiota to dietary changes in the first two years of life. Frontiers in pharmacology, 11, 334.
- ^ magazine, Ewen. "Microbial DNA in Human Body Can Be Used to Identify Individuals". Scientific American. Retrieved 2015-05-17.
- ^ Callaway, Ewen (2015). "Microbiomes raise privacy concerns". Nature. 521 (7551): 136. Bibcode:2015Natur.521..136C. doi:10.1038/521136a. PMID 25971486. S2CID 4393347.
- ^ Yong, Ed (2015-05-11). "Can The Microbes You Leave Behind Be Used to Identify You?". National Geographic. Archived from the original on May 30, 2015. Retrieved 2015-05-17.