Cerebral palsy patients do not exhibit the same motor impairments or postural problems but the common factor amongst all cerebral palsy cases is motor impairments resulting from brain defects or lesions [1].
Cerebral palsy is due to damage occurring to the developing brain.[2] This damage can occur during pregnancy, delivery, the first month of life, or less commonly in early childhood.[2] Structural problem in the brain are seen in 80% of cases, most commonly within the white matter.[2] While the exact causes are unclear, the events that lead to cerebral palsy may occur during pregnancy, delivery, the first month of life, or–less commonly–in early childhood.[2]
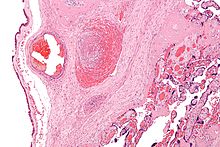
All the theories (see Figure 1) agree there is no single reason but instead a series of key events occur which eventually end in cerebral palsy. In other words, even if asphyxia or an infection happens, the end result will not always be cerebral palsy [3].

Possible Mechanisms During Birth
editDuring birth, asphyxia is the most common factor suspected to cause cerebral palsy [4]. An example of asphyxia during delivery is abruptio placenta (condition where the placenta separates from the uterus wall early). The resulting lack of oxygen to the fetal brain causes damage, which could lead to cerebral palsy [5].
Possible Mechanisms After Birth
editAfter birth, the predominant theory for causing cerebral palsy is infections damaging to the central nervous system. The central nervous system damage affects the fetal brain, which leads to cerebral palsy. Examples of infections would be pneumonia or meningitis [6].
Possible Mechanisms Before Birth
editThe most popular theory regarding the cause of cerebral palsy occurs before birth. The fetal inflammatory response syndrome (see Figure 2) proposes that when an infection occurs inside the uterus, the fetus responds by producing cytokines. These cytokines fight the infection but also have harmful effects on the fetal brain. The harmful effects might eventually result in cerebral palsy [7].
While in certain cases there is no identifiable cause, typical causes include problems in intrauterine development (e.g. exposure to radiation, infection), hypoxia of the brain, and birth trauma during labour and delivery, and complications around birth or during childhood.[8] More than three fourths of cases are believed to result from issues that occur during pregnancy.[2]
- ^ Reddihough, D. S. and Collins, K.J. (2003). “The Epidemiology and Causes of Cerebral Palsy.” Australian Journal of Physiotherapy, 49: 7-12
- ^ a b c d e Cite error: The named reference
Yar2013was invoked but never defined (see the help page). - ^ Reddihough, D. S. and Collins, K.J. (2003). “The Epidemiology and Causes of Cerebral Palsy.” Australian Journal of Physiotherapy, 49: 7-12
- ^ Schendel, D.E., Shuchat, A. and Thorsen, P (2002). “Public Health Issues Related to Infection in Pregnancy and Cerebral Palsy.” Mental Retardation and Developmental Disabilities Research Reviews, 8: 39-45
- ^ Yamada, T., Yamada, T., Morikawa, M. and Minakami, H. (2012). “Clinical Features of Abruptio Placentae as a Prominent Cause of Cerebral Palsy.” Early Human Development, 88: 861-864
- ^ Oval, F. (2010). “Perinatal Infections and Cerebral Palsy.” Journal of Pediatric Infectious Diseases, 5: 21 - 26
- ^ Bashiri, A., Burstein, E. and Mazor, M. (2006). “Cerebral Palsy and Fetal Inflammatory Response Syndrome: A Review.” Journal of Perinatal Medicine, 34: 5 – 12
- ^ Cite error: The named reference
CPBeukwas invoked but never defined (see the help page).
