| Langerhans cell histiocytosis | |
|---|---|
| Other names | Histiocytosis X[1] |
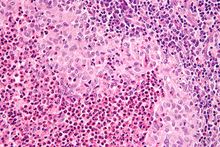 | |
| Micrograph showing a Langerhans cell histiocytosis with the characteristic reniform Langerhans cells accompanied by abundant eosinophils. H&E stain. | |
| Specialty | Hematology |
| Symptoms | Lesions in various tissues, fever, weight loss, diabetes insipidus, tiredness[1] |
| Types | Unifocal, chronic multifocal, multifocal multisystem, Hashimoto-Pritzker disease[2] |
| Diagnostic method | Tissue biopsy, medical imaging[2] |
| Treatment | None, surgery, radiation therapy, chemotherapy[2] |
| Prognosis | Variable[2] |
| Frequency | 1 to 2 per 100,000[3] |
Langerhans cell histiocytosis (LCH) is an abnormal increase in Langerhans immune cells from the bone marrow, which than migrate to the skin and other organs.[4] They can form a type of tumor, known as a granuloma.[4][5] Symptoms may include lesions in various tissues such as skin or bone, fever, weight loss, diabetes insipidus, or tiredness.[1]
LCH is due to a mutation in the MAPKinase pathway.[1] It is part of a group of syndromes called histiocytoses, which are characterized by an increased number of histiocytes (an old term for dendritic cells).[1][4] Diagnosis is confirmed by medical imaging and biopsy.[2] Blood tests may show low red blood cells, and occasionally low white blood cells and low platelets.[1] Many consider it a form of cancer, but there is still some disagreement.[2][6]
Mild cases may simple resolve on their own without treatment.[2] Otherwise treatment options may include some combination of surgery, radiation therapy, or chemotherapy.[2] LCH affects about 1 to 2 people per 100,000.[3] Most cases start in childhood;[3] though adults may also be affected.[4] Males are more commonly affected than females.[1] Hispanic people are more commonly affected.[1]
Evidence of the disease has been found in mummy dating back to 900-790. B.C.[7] LCH was previously known as "histiocytosis X".[8] Subtype include chronic multifocal LCH, previously known as "Hand–Schüller–Christian disease", unifocal LCH, previously known as "eosinophilic granuloma", multifocal multisystem LCH, previously known as "Letterer-Siwe disease", and Hashimoto-Pritzker disease.[2][9]
References edit
- ^ a b c d e f g h "Langerhans Cell Histiocytosis". NORD (National Organization for Rare Disorders). Archived from the original on 10 June 2021. Retrieved 5 December 2020.
- ^ a b c d e f g h i "Langerhans cell histiocytosis". rarediseases.info.nih.gov. National Institutes of Health. Archived from the original on 10 January 2021. Retrieved 6 December 2020.
- ^ a b c "Orphanet: Langerhans cell histiocytosis". www.orpha.net. Archived from the original on 28 August 2021. Retrieved 5 December 2020.
- ^ a b c d Payne, Jacqueline. "Langerhans' Cell Histiocytosis". patient.info. Archived from the original on 12 February 2012. Retrieved 6 December 2020. Last updated 28 Feb 2017.
- ^ Tebbi, Cameron K. (16 September 2020). Kanwar, Vikramjit S (ed.). "What is the Histiocyte Society classification of histiocytosis syndromes?". Medscape. Archived from the original on 20 January 2021. Retrieved 7 December 2020.
- ^ "Langerhans cell histiocytosis: MedlinePlus Genetics". medlineplus.gov. MedlinePlus. Archived from the original on 10 January 2021. Retrieved 6 December 2020.
- ^ Cavka, Mislav; Petaros, Anja; Ivanac, Gordana; Aganović, Lejla; Janković, Ivor; Reiter, Gert; Speier, Peter; Nielles-Vallespin, Sonja; Brkljacić, Boris (March 2012). "A probable case of Hand-Schueller-Christian's disease in an Egyptian mummy revealed by CT and MR investigation of a dry mummy". Collegium Antropologicum. 36 (1): 281–286. ISSN 0350-6134. PMID 22816232.
- ^ Broadbent, V.; Egeler, R. M.; Nesbit, M. E. (September 1994). "Langerhans cell histiocytosis--clinical and epidemiological aspects". The British Journal of Cancer. Supplement. 23: S11–S16. ISSN 0306-9443. PMC 2149699. PMID 8075001. Archived from the original on 2021-08-28. Retrieved 2020-12-06.
- ^ Pluot, Etienne; Davies, Mark; James, Steven L. J. (2009). "Who was who in bone tumours". In Davies, A. Mark; Sundaram, Murali; James, Steven J. (eds.). Imaging of Bone Tumors and Tumor-Like Lesions: Techniques and Applications. Springer. p. 681. ISBN 978-3-540-77982-7. Archived from the original on 2021-08-28. Retrieved 2020-12-06.