| Mr. Ibrahem/Crescentic glomerulonephritis | |
|---|---|
| Other names | Rapidly progressive glomerulonephritis (RPGN)[1] |
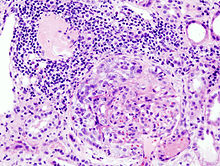 | |
| Histopathological image of crescentic glomerulonephritis in a person with MPO-ANCA positive rapid progressive glomerulonephritis. Hematoxylin & eosin stain. | |
| Specialty | Nephrology |
| Symptoms | Bloody urine, foamy urine, swelling, fever, abdominal pain[2][3] |
| Complications | Kidney failure[3] |
| Usual onset | 20 to 50 years old[3] |
| Causes | Anti-glomerular basement membrane disease, granulomatosis with polyangiitis, microscopic polyangiitis, following infection, lupus nephritis, IgA nephropathy[3] |
| Diagnostic method | Blood tests, urine tests, and kidney biopsy[2] |
| Differential diagnosis | Other causes of acute kidney injury, nephrotic syndrome[2] |
| Treatment | Corticosteroids, plasmapheresis, dialysis[2][3] |
| Prognosis | Better with early treatment[3] |
| Frequency | Rare[2] |
Crescentic glomerulonephritis, previously known as rapidly progressive glomerulonephritis, is combination of a rapid decrease in kidney function, blood and protein in the urine, and specific findings on kidney biopsy.[2] Other symptoms may include tiredness, joint pain, fever, swelling, and abdominal pain.[3] Without treatment, kidney failure occurs within weeks to months.[3]
It may occur as a result of anti-glomerular basement membrane disease, granulomatosis with polyangiitis, microscopic polyangiitis, lupus nephritis, IgA nephropathy, and following infection.[3] Diagnosis is based on blood tests, urine tests, and a kidney biopsy.[2] The biopsy show crescent-shaped scaring in over half the glomeruli.[3]
Initial treatment is generally with intravenous methylprednisolone.[2] Further treatment may depend on the underlying cause.[2] Other medications that may be used include cyclophosphamide or rituximab.[3] Plasmapheresis may be considered if their is lung involvement.[2] Kidney failure may be treated with dialysis or kidney transplant.[3]
Crescentic glomerulonephritis is rare, occurring in about 2 to 7 people per million per year.[2] Those affected are generally between 20 to 50 years of age.[3] Males and females are affected equally frequently.[2] White people are more commonly affected.[2] The underlying appearance on kidney biopsy was first described in 1914 while the current name came into use in 1942.[4]
References
edit- ^ "Orphanet: OBSOLETE: Rapidly progressive glomerulonephritis". www.orpha.net. Archived from the original on 3 May 2020. Retrieved 25 January 2021.
- ^ a b c d e f g h i j k l m Naik, RH; Shawar, SH (January 2020). "Rapidly Progressive Glomerulonephritis". StatPearls. PMID 32491362.
- ^ a b c d e f g h i j k l m "Rapidly Progressive Glomerulonephritis (RPGN) - Genitourinary Disorders". Merck Manuals Professional Edition. Archived from the original on 25 November 2020. Retrieved 25 January 2021.
- ^ Visveswaran, kasi (2009). Essentials of Nephrology, 2/e. BI Publications Pvt Ltd. p. 98. ISBN 978-81-7225-323-3. Archived from the original on 2021-08-28. Retrieved 2021-01-25.