The pigmented layer of retina or retinal pigment epithelium (RPE) is the pigmented cell layer just outside the neurosensory retina that nourishes retinal visual cells, and is firmly attached to the underlying choroid and overlying retinal visual cells.[1][2]
| Retinal pigment epithelium | |
|---|---|
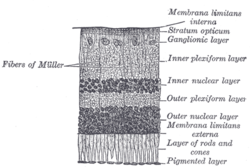 Section of retina. (Pigmented layer labeled at bottom right.) | |
 Plan of retinal neurons. (Pigmented layer labeled at bottom right.) | |
| Details | |
| Identifiers | |
| Latin | stratum pigmentosum retinae, pars pigmentosa retinae |
| MeSH | D055213 |
| TA98 | A15.2.04.008 |
| TA2 | 6782 |
| FMA | 58627 |
| Anatomical terminology | |
History
editThe RPE was known in the 18th and 19th centuries as the pigmentum nigrum, referring to the observation that the RPE is dark (black in many animals, brown in humans); and as the tapetum nigrum, referring to the observation that in animals with a tapetum lucidum, in the region of the tapetum lucidum the RPE is not pigmented.[3]
Anatomy
editThe RPE is composed of a single layer of hexagonal cells that are densely packed with pigment granules.[1]
When viewed from the outer surface, these cells are smooth and hexagonal in shape. When seen in section, each cell consists of an outer non-pigmented part containing a large oval nucleus and an inner pigmented portion which extends as a series of straight thread-like processes between the rods, this being especially the case when the eye is exposed to light.
Function
editThe RPE has several functions,[4] namely, light absorption, epithelial transport, spatial ion buffering, visual cycle, phagocytosis, secretion and immune modulation.
- Light absorption: RPE are responsible for absorbing scattered light. This role is very important for two main reasons, first, to improve the quality of the optical system, second, light is radiation, and it is concentrated by a lens onto the cells of the macula, resulting in a strong concentration of photo-oxidative energy. Melanosomes absorb the scattered light and thus diminish the photo-oxidative stress. The high perfusion of retina brings a high oxygen tension environment. The combination of light and oxygen brings oxidative stress, and RPE has many mechanisms to cope with it.
- Epithelial transport: As mentioned above, RPE compose the outer blood–retinal barrier, the epithelia has tight junctions between the lateral surfaces and implies an isolation of the inner retina from the systemic influences. This is important for the immune privilege (not only as barrier, but with signalling process as well) of eyes, a highly selective transport of substances for a tightly controlled environment. RPE supply nutrients to photoreceptors, control ion homeostasis and eliminate water and metabolites.
- Spatial buffering of ions: Changes in the subretinal space are fast and require a capacitative compensation by RPE[5] many cells are involved in transduction of light and if they are not compensated for, they are no longer excitable and proper transduction would not be possible. The normal transepithelial transport of ions would be too slow to compensate quickly enough for these changes, there are many underlying mechanisms based on the activity of voltage-dependent ion channels add to the basic transepithelial transport of ions.[6]
- Visual cycle: The visual cycle fulfills an essential task of maintaining visual function and needs therefore to be adapted to different visual needs such as vision in darkness or lightness. For this, functional aspects come into play: the storage of retinal and the adaption of the reaction speed. Basically, vision at low light intensities requires a lower turn-over rate of the visual cycle, whereas in well-lit conditions the turn-over rate is much higher. In the sudden transition from darkness to light, a large amount of 11-cis retinal is required. This comes not directly from the visual cycle but from several retinal pools of retinal binding proteins which are connected to each other by the transportation and reaction steps of the visual cycle.
- Phagocytosis of photoreceptor outer segment (POS) membranes: POS are exposed to constant photo-oxidative stress, and they go through constant destruction by it. They are constantly renewed by shedding their end, which RPE then phagocytose and digest.
- Secretion: The RPE is an epithelium which closely interacts with photoreceptors on one side but must also be able to interact with cells on the blood side of the epithelium, such as endothelial cells or cells of the immune system. In order to communicate with the neighboring tissues the RPE is able to secrete a large variety of factors and signaling molecules. It secretes ATP, fas-ligand (fas-L), fibroblast growth factors (FGF-1, FGF-2, and FGF-5), transforming growth factor-β (TGF-β), insulin-like growth factor-1 (IGF-1), ciliary neurotrophic factor (CNTF), platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), lens epithelium-derived growth factor (LEDGF), members of the interleukin family, tissue inhibitor of matrix metalloproteinase (TIMP) and pigment epithelium-derived factor (PEDF). Many of these signaling molecules have important physiopathologic roles.
- Immune privilege of the eye: The inner eye represents an immune privileged space which is disconnected from the immune system of the blood stream. The immune privilege is supported by the RPE in two ways. First, it represents a mechanical and tight barrier which separates the inner space of the eye from the blood stream. Second, the RPE is able to communicate with the immune system in order to silence immune reaction in the healthy eye or, on the other hand, to activate the immune system in the case of disease.
Pathology
editIn the eyes of albinos, the cells of this layer contain no pigment. Dysfunction of the RPE is found in age-related macular degeneration[7][8] and retinitis pigmentosa. RPE are also involved in diabetic retinopathy. Gardner syndrome is characterized by FAP (familial adenomatous polyps), osseous and soft tissue tumors, retinal pigment epithelium hypertrophy and impacted teeth.[9]
See also
editReferences
editThis article incorporates text in the public domain from page 1016 of the 20th edition of Gray's Anatomy (1918)
- ^ a b Cassin, B. & Solomon, S. (2001). Dictionary of eye terminology. Gainesville, Fla: Triad Pub. Co. ISBN 0-937404-63-2.
- ^ Boyer MM, Poulsen GL, Nork TM. "Relative contributions of the neurosensory retina and retinal pigment epithelium to macular hypofluorescence." Arch Ophthalmol. 2000 Jan; 118(1):27–31. PMID 10636410.
- ^ Coscas, Gabriel & Felice Cardillo Piccolino (1998). Retinal Pigment Epithelium and Macular Diseases. Springer. ISBN 0-7923-5144-4.
- ^ Strauss O (2005) "The retinal pigment epithelium in visual function". Physiol Rev 85:845–81
- ^ Steinberg RH, Linsenmeier RA, Griff ER (1983) "Three light-evoked responses of the retinal pigment epithelium". Vision Res 23:1315–23
- ^ Baylor D (1996) "How photons start vision". Proc Natl Acad Sci 93:560–65
- ^ Naik, Gautam (14 October 2014). "Stem Cells Show Potential Benefits for Eye Diseases". Wall Street Journal.
- ^ Regalado, Antonio (October 15, 2014). "Stem Cells Pass Eye Safety Test". MIT Technology Review.
- ^ "UpToDate". www.uptodate.com.
Further reading
edit- Spaide, RF; Curcio, CA (September 2011). "Anatomical correlates to the bands seen in the outer retina by optical coherence tomography: literature review and model". Retina (Philadelphia, Pa.). 31 (8): 1609–19. doi:10.1097/IAE.0b013e3182247535. PMC 3619110. PMID 21844839.
- Yang, Song; Zhou, Jun; Li, Dengwen (28 July 2021). "Functions and Diseases of the Retinal Pigment Epithelium". Frontiers in Pharmacology. 12: 727870. doi:10.3389/fphar.2021.727870. PMC 8355697. PMID 34393803.
External links
edit- pigment+epithelium+of+eye at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Histology image: 07902loa – Histology Learning System at Boston University
- Histology at KUMC eye_ear-eye11