Unstable angina is a type of angina pectoris[1] that is irregular or more easily provoked.[2] It is classified as a type of acute coronary syndrome.[3]
| Unstable angina | |
|---|---|
| Other names | Crescendo angina |
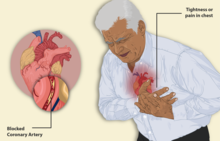 | |
| Illustration depicting angina | |
| Specialty | Cardiology |
| Symptoms | Chest pain or chest discomfort at rest or minimal exertion, or a new onset chest pain or discomfort on exertion. |
| Complications | Coronary artery disease |
It can be difficult to distinguish unstable angina from non-ST elevation (non-Q wave) myocardial infarction.[4][5] They differ primarily in whether the ischemia is severe enough to cause sufficient damage to the heart's muscular cells to release detectable quantities of a marker of injury, typically troponin T or troponin I.[4][6] Unstable angina is considered to be present in patients with ischemic symptoms suggestive of an acute coronary syndrome and no change in troponin levels, with or without changes indicative of ischemia (e.g., ST segment depression or transient elevation or new T wave inversion) on electrocardiograms.[4]
Signs and symptoms
editSymptoms of unstable angina are the same as those of stable angina, however the pattern of the symptoms changes.[7] In unstable angina, symptoms related to decreased blood flow to the heart may appear on rest or on minimal exertion.[4] The symptoms can last longer than those in stable angina, can be resistant to rest or medicine, and can get worse over time.[7][8]
The cardinal symptom of critically decreased blood flow to the heart is chest pain, experienced as tightness, pressure, or burning.[5] Localisation is most commonly around or over the chest and may radiate or be located to the arm, shoulder, neck, back, upper abdomen, or jaw.[5] This may be associated with sweating, nausea, or shortness of breath.[5] Previously the word "atypical" was used to describe chest pain not typically heart-related; however, this word is recommended against and has been replaced by "noncardiac" to describe chest pain that indicate a low likelihood of heart-related pain.[5]
Pathophysiology
editThe pathophysiology of unstable angina is controversial. Previously, unstable angina was assumed to be angina pectoris caused by disruption of an atherosclerotic plaque with partial thrombosis and possibly embolization or vasospasm leading to myocardial ischemia.[9][10] However, sensitive troponin assays reveal rise of cardiac troponin in the bloodstream with episodes of even mild myocardial ischemia.[11] Since unstable angina is assumed to occur in the setting of acute myocardial ischemia without troponin release, the concept of unstable angina is being questioned with some calling for retiring the term altogether.[12]
Diagnosis
editUnstable angina is characterized by at least one of the following:
- Occurs at rest or minimal exertion and usually lasts more than 20 minutes (if nitroglycerin is not administered)
- Being severe (at least Canadian Cardiovascular Society Classification 3) and of new onset (i.e. within 1 month)
- Occurs with a crescendo pattern (brought on by less activity, more severe, more prolonged or increased frequency than previously).[13][14][15]
Fifty percent of people with unstable angina will have evidence of necrosis of the heart's muscular cells based on elevated cardiac serum markers such as creatine kinase isoenzyme (CK)-MB and troponin T or troponin I, and thus have a diagnosis of non-ST elevation myocardial infarction.[15][16]
Management
editNitroglycerin can be used immediately to dilate the venous system and reduce the circulating blood volume, therefore reducing the work and oxygen demand of the heart.[17][18] In addition, nitroglycerin causes peripheral venous and artery dilation reducing cardiac preload and afterload. These reductions allow for decreased stress on the heart and therefore lower the oxygen demand of the heart's muscle cells.[19]
Antiplatelet drugs such as aspirin and clopidogrel can reduce platelet aggregation at the unstable atherosclerotic plaque, as well as combining these with an anticoagulant such as a low molecular weight heparin, can reduce clot formation.[20]
See also
editReferences
edit- ^ Yeghiazarians Y, Braunstein JB, Askari A, Stone PH (January 2000). "Unstable angina pectoris". N. Engl. J. Med. 342 (2): 101–14. doi:10.1056/NEJM200001133420207. PMID 10631280.
- ^ "unstable angina" at Dorland's Medical Dictionary
- ^ Wiviott, S. D.; Braunwald, E (2004). "Unstable Angina and Non–ST-Segment Elevation Myocardial Infarction: Part I. Initial Evaluation and Management, and Hospital Care". American Family Physician. 70 (3): 525–32. PMID 15317439.
- ^ a b c d Collet, Jean-Philippe; Thiele, Holger; Barbato, Emanuele; Barthélémy, Olivier; Bauersachs, Johann; et al. (2021-04-07). "2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation". European Heart Journal. 42 (14): 1289–1367. doi:10.1093/eurheartj/ehaa575. ISSN 1522-9645. PMID 32860058.
Unstable angina is defined as myocardial ischaemia at rest or on minimal exertion in the absence of acute cardiomyocyte injury/necrosis. [...] Compared with NSTEMI patients, individuals with unstable angina do not experience acute cardiomyocyte injury/necrosis.
- ^ a b c d e Gulati, Martha; Levy, Phillip D.; Mukherjee, Debabrata; Amsterdam, Ezra; Bhatt, Deepak L.; et al. (2021-11-30). "2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines". Circulation. 144 (22): e368–e454. doi:10.1161/CIR.0000000000001029. ISSN 0009-7322. PMID 34709879.
- ^ Barthélémy, Olivier; Jobs, Alexander; Meliga, Emanuele; et al. (2021-04-07). "Questions and answers on workup diagnosis and risk stratification: a companion document of the 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation". European Heart Journal. 42 (14): 1379–1386. doi:10.1093/eurheartj/ehaa602. ISSN 1522-9645. PMC 8026278. PMID 32860030.
NSTEMI is characterized by ischaemic symptoms associated with acute cardiomyocyte injury (=rise and/or fall in cardiac troponin T/I), while ischaemic symptoms at rest (or minimal effort) in the absence of acute cardiomyocyte injury define unstable angina. This translates into an increased risk of death in NSTEMI patients, while unstable angina patients are at relatively low short-term risk of death.
- ^ a b "Acute Coronary Syndromes (Heart Attack; Myocardial Infarction; Unstable Angina) - Heart and Blood Vessel Disorders". MSD Manual Consumer Version. Retrieved 2023-02-12.
- ^ "Unstable Angina". www.heart.org. American Heart Association. Archived from the original on 2023-03-15. Retrieved 2023-05-05.
- ^ Robbins (2005). Pathologic Basis of Disease (7th ed.).
- ^ Braunwald, E. (1998). "Unstable Angina: An Etiologic Approach to Management". Circulation. 98 (21): 2219–2222. doi:10.1161/01.CIR.98.21.2219. PMID 9826306.
- ^ Sabatine, M. S.; Morrow, R. W.; de Lemos, J.A.; Jarolim, P.; Braunwald, E. (2009). "Detection of acute changes in circulating troponin in the setting of transient stress test-induced myocardial ischaemia using an ultrasensitive assay: results from TIMI 35". European Heart Journal. 30 (2): 162–169. doi:10.1093/eurheartj/ehn504. PMC 2721709. PMID 18997177.
- ^ Braunwald, E.; Morrow, R. W. (2013). "Unstable Angina. Is It Time for a Requiem?". Circulation. 127 (24): 2452–2457. doi:10.1161/CIRCULATIONAHA.113.001258. PMID 23775194.
- ^ Robert A., Chahine (1975). "Unstable angina The problem of definition" (PDF). British Heart Journal. 37 (12): 1246–1249. doi:10.1136/hrt.37.12.1246. PMC 482947. PMID 1225338.
- ^ Braunwald, E; et al. (2002). "ACC/AHA guideline update for the management of patients with unstable angina and non-ST segment elevation myocardial infarction-2002: Summary Article: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients with Unstable Angina)". Circulation. 106 (14): 1893–1900. doi:10.1161/01.cir.0000037106.76139.53. PMID 12356647.
- ^ a b Libby: Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine
- ^ Markenvard, J; Dellborg, M; Jagenburg, R; Swedberg, K (1992). "The predictive value of CKMB mass concentration in unstable angina pectoris: preliminary report". Journal of Internal Medicine. 231 (4): 433–6. doi:10.1111/j.1365-2796.1992.tb00956.x. PMID 1588271. S2CID 32268852.
- ^ Murrell, William (1879). "Nitroglycerin as a remedy for angina pectoris". The Lancet. 1 (2890): 80–81, 113–115, 151–152, 225–227. doi:10.1016/s0140-6736(02)46032-1. hdl:2027/uc1.b5295238. PMC 5901592.
- ^ Sneader, Walter (2005). Drug Discovery: A History. John Wiley and Sons. ISBN 978-0-471-89980-8.
- ^ Boden, William E.; Padala, Santosh K.; Cabral, Katherine P.; Buschmann, Ivo R.; Sindhu, Mandeep S. (2015). "Role of short-acting nitroglycerin in the management of ischemic heart disease". Drug Design, Development and Therapy. 9: 4793–805. doi:10.2147/DDDT.S79116. PMC 4548722. PMID 26316714.
- ^ Robert, Chahine (1975). "Unstable angina" (PDF). British Heart Journal. 37 (12): 1246–1249. doi:10.1136/hrt.37.12.1246. PMC 482947. PMID 1225338.