| Hypopituitarism | |
|---|---|
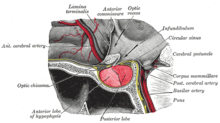 | |
| The pituitary gland on a plate from Gray's Anatomy (1918). The anterior lobe is on the left, and the posterior lobe on the right, both in red. | |
| Specialty | Endocrinology |
| Symptoms | Adrenal insufficiency, hypothyroidism, hypogonadism, GH deficiency, ADH deficiency, vision loss, headaches[1] |
| Usual onset | Gradual or sudden[2] |
| Causes | Pituitary tumors, tumors near the pituitary, pituitary apoplexy, traumatic brain injury, pituitary surgery or radiation therapy, hypophysitis[1] |
| Diagnostic method | Blood tests, medical imaging[1] |
| Treatment | Depends on the underlying cause and missing hormones[1] |
| Medication | Thyroxine, hydrocortisone, sex steroids, growth hormone, desmopressin[2] |
| Prognosis | Usually good with treatment[2][1] |
| Frequency | 1 in 2,000 (Spain)[1] |
Hypopituitarism is the decreased secretion of one or more of the eight hormones normally produced by the pituitary gland at the base of the brain.[2] Symptoms vary, depending on which hormones are involved and on the underlying cause.[1] These may include adrenal insufficiency, hypothyroidism, hypogonadism, GH deficiency, ADH deficiency, vision loss, and headaches.[1] Onset can be gradual or sudden.[2]
Causes include pituitary tumors (60%), tumors near the pituitary, pituitary apoplexy, traumatic brain injury, pituitary surgery or radiation therapy, and hypophysitis.[1] In about 10% of cases the cause is unknown.[3] Diagnosis is often based on blood tests looking at hormone levels and medical imaging.[1] The deficiency of one hormone is known as selective hypopituitarism while if most or all are decreased, the term panhypopituitarism is used.[4]
Treatment in part depends on the underlying cause.[1] Most hormones can be replaced by tablets or injections such as with thyroxine, hydrocortisone, sex steroids, growth hormone, or desmopressin.[2] If of sudden onset, rapid cortisol replacement is key.[2] While it is associated with an increased risk of death, outcomes are usually good with treatment.[2][1]
Hypopituitarism is estimated to affect 1 in 2,000 people in Spain.[1] It may also be underdiagnosed in people with previous traumatic brain injury.[3] The condition was first described in 1914 by the German physician Morris Simmonds.[5][6]
References edit
- ^ a b c d e f g h i j k l m Gounden, V; Jialal, I (January 2021). "Hypopituitarism". PMID 29262053.
{{cite journal}}: Cite journal requires|journal=(help) - ^ a b c d e f g h Higham, CE; Johannsson, G; Shalet, SM (12 November 2016). "Hypopituitarism". Lancet (London, England). 388 (10058): 2403–2415. doi:10.1016/S0140-6736(16)30053-8. PMID 27041067.
- ^ a b Schneider HJ, Aimaretti G, Kreitschmann-Andermahr I, Stalla GK, Ghigo E (April 2007). "Hypopituitarism". Lancet. 369 (9571): 1461–70. doi:10.1016/S0140-6736(07)60673-4. PMID 17467517. S2CID 208789791.
- ^ Lewis, Sharon L.; Bucher, Linda; Heitkemper, Margaret M.; Harding, Mariann M.; Kwong, Jeffrey; Roberts, Dottie (2016). Medical-Surgical Nursing - E-Book: Assessment and Management of Clinical Problems, Single Volume. Elsevier Health Sciences. p. 1158. ISBN 978-0-323-37143-8.
- ^ Simmonds (1914). "Über hypophysisschwund mit todlichem ausgang". Dtsch Med WSCHR. 40 (7): 322–323. doi:10.1055/s-0029-1190185.
- ^ Bynum, W. F.; Porter, Roy (2013). Companion Encyclopedia of the History of Medicine. Routledge. p. 501. ISBN 978-1-136-11036-8.