Pseudohypoaldosteronism (PHA) is a condition that mimics hypoaldosteronism.[1]
| Pseudohypoaldosteronism Type 1 | |
|---|---|
 | |
| In pseudohypoaldosteronism type 1, aldosterone is elevated (hyperaldosteronism), but because the body fails to respond to it, it appears similar to hypoaldosteronism. | |
| Specialty | Nephrology |
| Symptoms | Failure to thrive, dehydration, hyponatremia, metabolic acidosis, hyperkalemia, and other non-specific symptoms including nausea, vomiting, extreme fatigue, and muscle weakness. |
| Causes | Mutations in the MLR, NR3C2, SCNN1A, SCNN1B, or SCNN1G genes |
Pseudohypoaldosteronism Type 1 (PHA1) edit
Pseudohypoaldosteronism type 1 (PHA1) is characterized by the body's inability to respond adequately to aldosterone, a hormone crucial for regulating electrolyte levels. This condition often manifests with dehydration as the kidneys struggle to retain sufficient salt, leading to symptoms like increased thirst and dry mouth. Additionally, PHA1 disrupts electrolyte balance, resulting in high levels of sodium and low levels of potassium in the blood.
Mechanism edit
This section is empty. You can help by adding to it. (March 2024) |
Onset edit
This section is empty. You can help by adding to it. (March 2024) |
Symptoms edit
This section is empty. You can help by adding to it. (March 2024) |
Types edit
| Type | OMIM | Gene | Inheritance | Age of Onset | Description |
|---|---|---|---|---|---|
| PHA1A | 177735 | MLR, NR3C2 | Autosomal dominant | Neonatal but improves with age. Adults are usually asymptomatic without treatment. | Salt wasting caused by renal unresponsiveness to mineralocorticoids. Patients often present with hyperkalaemic acidosis despite high aldosterone levels. Not all individuals with the mutation develop PHA1A suggesting that illness and volume depletion may play a role in the development of the clinically recognized PHA1A. |
| PHA1B | 264350 | SCNN1A, SCNN1B, SCNN1G of the epithelial sodium channel | Autosomal recessive | Neonatal, appears to become less aggressive with age | Renal salt wasting and high concentrations of sodium in sweat, stool, and saliva. The disorder often involves multiple organ systems and can be life threatening in the neonatal period. Patients usually present with hyponatremia, hyperkalemia, and increased plasma renin activity with high serum aldosterone concentrations. PHA1B is often mistaken for cystic fibrosis. |
Treatment edit
Treatment of severe forms of PHA1 requires relatively large amounts of sodium chloride.[2] These conditions also involve hyperkalemia.[3]
Risks edit
Individuals with PHA1B can have additional symptoms such as cardiac arrhythmia, shock, recurrent lung infections, or lesions on the skin due to imbalanced salts in the body especially in infancy.
A stop mutation in the SCNN1A gene has been shown to be associated with female infertility.[4]
Pseudohypoaldosteronism Type 2 (PHA2) edit
PHA2 also known as Familial hyperkalemic hypertension or Gordon syndrome is a rare disorder characterized by abnormalities in how the body regulates sodium and potassium levels. This condition stems from mutations in specific genes involved in sodium transport within the kidneys.
Unlike in PHA1 in which aldosterone resistance is present, in PHA2 blood volume increases occur regardless of normal or low aldosterone levels due to the enhanced activity of sodium transporters in the kidney.[5]
Mechanism edit
PHA2 is associated with mutations in the WNK4, WNK1, KLHL3 and CUL3 genes. These genes regulate the Sodium-chloride symporter (NCC) transporter, which is involved in controlling the levels of sodium and chloride in the body. Normally, the NCC transporter helps reabsorb sodium and chloride in a part of the kidney called the distal convoluted tubule (DCT), however in PHA2 this process is disrupted. Mutations in these genes lead to overactivity of NCC, causing excessive sodium and chloride reabsorption.
Mutations in KLHL3 and WNK4 are also known to create an overactivity in ENaC. EnaC is responsible for sodium and water reabsorption in the kidney. An overactiveity in ENaC can result in sodium wasting similar to PHA1.[6]
The hyperkalemia found in PHA2 is proposed to be a function of diminished sodium delivery to the cortical collecting tubule (potassium excretion is mediated by the renal outer medullary potassium channel (ROMK) in which sodium reabsorption plays a role). Alternatively, WNK4 mutations that result in a gain of function of the Na-Cl co-transporter may inhibit ROMK activity resulting in hyperkalemia.[7]
Onset edit
The age of onset is difficult to pinpoint and can range from infancy to adulthood.
Symptoms edit
People with PHA2 have hypertension and hyperkalemia despite having normal kidney function. Many individuals with PHA2 will develop hyperkalemia first, and will not present with hypertension until later in life. They also commonly experience both hyperchloremia and metabolic acidosis together, a condition called hyperchloremic metabolic acidosis.
People with PHA2 may experience other nonspecific symptoms including nausea, vomiting, extreme fatigue, muscle weakness, and hypercalcuria.
Some PHA2E patients present with dental abnormalities.[8] Patients with recessive KLHL3 mutations and dominant CUL3 mutations tend to have more severe phenotypes.[9]
A study in 2024 linked PHA2 to epilepsy. Epileptic seizures were seen in 3 of the 44 affected subjects. Two of the subjects had Generalized tonic–clonic seizure and one subject had migraine seizures. All three subjects had WNK4 mutations. It's speculated that the epilepsy may be caused by potassium spikes resulting in abnormal CNS neuron activity. The study also linked PHA2 to Proximal Renal Tubular Acidosis.[10] Metabolic acidosis is also known to cause epileptic seizures.
Types edit
| Type | OMIM | Gene | Inheritance | Age Of Onset | Description |
|---|---|---|---|---|---|
| PHA2A | 145260 | mapped to chromosome 1q31-q42[11] | Autosomal dominant | Varies | Does not involve salt wasting. |
| PHA2B | 614491 | WNK4 | Autosomal dominant | 10+ with a mean age of 28[12] | May involve salt wasting.[6] Patients typically do not experience hypertension until adulthood.[12] Bicarbonate is higher than other PHA2 types. Aldosterone concentrations are often normal.[13] TRPV6 may be involved.[14] |
| PHA2C | 614492 | WNK1 | Autosomal dominant | 15+ with a mean age of 36[12] | Does not involve salt wasting.[6] Significantly less severely affected than other PHA2 types.[12] Affected patients have hypertension together with long-term hyperkalemia, hyperchloremia, normal plasma creatinine, reduced bicarbonate, and low renin levels. Aldestrone levels may be normal or elevated. |
| PHA2D | 614495 | KLHL3 | Autosomal dominant or Autosomal recessive | Mean age at diagnosis was found to be around 24 to 26, but it varies widely.[12] | May involve salt wasting.[6] Individuals with the autosomal dominant mutations typically show higher potassium levels than those with autosomal recessive mutations. Hypertension usually develops in adulthood. Patients often present with low bicarbonate (17-18).[12] |
| PHA2E | 614496 | CUL3 | Autosomal dominant | 3-15 years old[12] | Most severe manifestations of PHA2 compared to patients with other mutations. Almost all individuals present with hypertension before age 18.[12] |
Treatment edit
PHA2 requires salt restriction and use of thiazide diuretics to block sodium chloride reabsorption and normalise blood pressure and serum potassium.[citation needed]
Risks edit
Pregnancy Risks edit
As of 2018, at least 7 reported cases of severe metabolic acidosis occurring during pregnancy have been reported in PHA2 patients.[15]
A study in 2023 also described a patient with severe preeclampsia later being diagnosed with PHA2D. The twin babies born healthy and discharged from the hospital.[16]
Other Risks edit
One study noted that severe hypercalciuria from untreated PHA2 resulted in kidney stones, and osteoporosis in some patients.[17]
History edit
This syndrome was first described by Cheek and Perry in 1958.[18] Later pediatric endocrinologist Aaron Hanukoglu reported that there are two independent forms of PHA with different inheritance patterns: A renal form with autosomal dominant inheritance exhibiting salt loss mainly from the kidneys, and a multi-system form with autosomal recessive form exhibiting salt loss from kidney, lung, and sweat and salivary glands.[19][20]
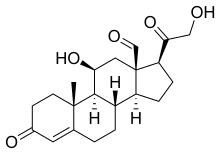
The hereditary lack of responsiveness to aldosterone could be due to at least two possibilities: 1. A mutation in the mineralocorticoid receptor that binds aldosterone, or 2. A mutation in a gene that is regulated by aldosterone. Linkage analysis on patients with the severe form of PHA excluded the possibility of linkage of the disease with the mineralocorticoid receptor gene region.[21] Later, the severe form of PHA was discovered to be due to mutations in the genes SCNN1A, SCNN1B, and SCNN1G that code for the epithelial sodium channel subunits, α, β, and γ, respectively.[22]
See also edit
References edit
- ^ "Pseudohypoaldosteronism: Overview - eMedicine Pediatrics: General Medicine". Retrieved 2009-03-06.
- ^ Hanukoglu A, Hanukoglu I (2010). "Clinical improvement in patients with autosomal recessive pseudohypoaldosteronism and the necessity for salt supplementation". Clinical and Experimental Nephrology. 14 (5): 518–519. doi:10.1007/s10157-010-0326-8. PMID 20661616. S2CID 9764720.
- ^ Pseudohypoaldosteronism at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- ^ Boggula VR, Hanukoglu I, Sagiv R, Enuka Y, Hanukoglu A (October 2018). "Expression of the epithelial sodium channel (ENaC) in the endometrium - Implications for fertility in a patient with pseudohypoaldosteronism". The Journal of Steroid Biochemistry and Molecular Biology. 183: 137–141. doi:10.1016/j.jsbmb.2018.06.007. PMID 29885352. S2CID 47010706.
- ^ O'Shaughnessy, Kevin M. (November 2015). "Gordon Syndrome: a continuing story". Pediatric Nephrology (Berlin, Germany). 30 (11): 1903–1908. doi:10.1007/s00467-014-2956-7. ISSN 1432-198X. PMID 25503323. S2CID 195676310.
- ^ a b c d Susa, Koichiro (2014). "Impaired degradation of WNK1 and WNK4 kinases causes PHAII in mutant KLHL3 knock-in mice". Human Molecular Genetics. 23 (19): 5052–506. doi:10.1093/hmg/ddu217. PMID 24821705.
- ^ Garovic, Vesna D. (2006). "Monogenic Forms of Low-Renin Hypertension". Nature Clinical Practice. Nephrology. 2 (11). Nature Clinical Practice Nephrology: 624–30. doi:10.1038/ncpneph0309. PMID 17066054. S2CID 27864633. Retrieved 18 October 2019.
- ^ Nagahara, Keiko (December 2015). "Evaluation of Phosphorylated Urinary Na-Cl Cotransporter Is Potentially Useful in a Patient With Pseudohypoaldosteronism Type II due to Mutation in CUL3". Journal of the American Society of Nephrology. 27 (8): 2309–2318. doi:10.1681/ASN.2015020154. PMC 4978035. PMID 26701978.
- ^ Fernandez, Cornelius J. (2023). Monogenic hypertension with hyperkalemic acidosis, low renin, and variable aldosterone. pp. 1–117. doi:10.1016/C2021-0-01825-3. ISBN 978-0-323-96120-2.
- ^ Shirin, Neta (2024). "Association of Familial Hyperkalemia and Hypertension with Proximal Renal Tubular Acidosis and Epileptic Seizures". Nephron. 3 (148): 179–184. doi:10.1159/000531868. PMID 37666233.
- ^ Mansfield, Traci A. (1997). "Multilocus linkage of familial hyperkalaemia and hypertension, pseudohypoaldosteronism type II, to chromosomes 1q31-42 and 17p11-q21". Nat Genet. 16 (2): 202–205. doi:10.1038/ng0697-202. PMID 9171836.
- ^ a b c d e f g h Boyden, Lynn M (2012). "Mutations in kelch-like 3 and cullin 3 cause hypertension and electrolyte abnormalities". Nature. 482 (7383): 98–102. Bibcode:2012Natur.482...98B. doi:10.1038/nature10814. PMC 3278668. PMID 22266938.
- ^ Farfel, Zvi (1978). "Proximal Renal Tubular Acidosis Association With Familial Normaldosteronemic Hyperpotassemia and Hypertension". Arch Intern Med. 138 (12): 1837–1840. doi:10.1001/archinte.1978.03630370047021. PMID 718349.
- ^ Yang SS, Hsu YJ, Chiga M, Rai T, Sasaki S, Uchida S, Lin SH (Apr 2010). "Mechanisms for hypercalciuria in pseudohypoaldosteronism type II-causing WNK4 knock-in mice". Endocrinology. 151 (4): 1829–36. doi:10.1210/en.2009-0951. PMID 20181799.
- ^ Awad, Sara (2018). "Resolution of Metabolic Abnormalities During Pregnancy in a Patient with Gordon Syndrome and KLHL3 Mutation". AACE Clinical Case Reports. 4 (3): 235–239. doi:10.4158/AACR-2017-0006.
- ^ Taylor, Cater (2023). "Pseudohypoaldosteronism Type 2: A New Variant Of A Rare Disease". Journal of the Endocrine Society. doi:10.1210/jendso/bvad114 (inactive 2024-04-07).
{{cite journal}}: CS1 maint: DOI inactive as of April 2024 (link) - ^ D’ambrosio, Viola (June 2023). "#6875 Complications and Treatment of Hypercalciuria in Familial Hyperkalaemic Hypertension (FHHT)". Nephrology Dialysis Transplantation. 38 (1). doi:10.1093/ndt/gfad063c_6875.
- ^ CHEEK DB, PERRY JW (1958). "A salt wasting syndrome in infancy". Arch Dis Child. 33 (169): 252–6. doi:10.1136/adc.33.169.252. PMC 2012226. PMID 13545877.
- ^ Hanukoglu A (Nov 1991). "Type I pseudohypoaldosteronism includes two clinically and genetically distinct entities with either renal or multiple target organ defects". The Journal of Clinical Endocrinology and Metabolism. 73 (5): 936–44. doi:10.1210/jcem-73-5-936. PMID 1939532.
- ^ Hanukoglu I, Hanukoglu A (Jan 2016). "Epithelial sodium channel (ENaC) family: Phylogeny, structure-function, tissue distribution, and associated inherited diseases". Gene. 579 (2): 95–132. doi:10.1016/j.gene.2015.12.061. PMC 4756657. PMID 26772908.
- ^ Chung E, Hanukoglu A, Rees M, Thompson R, Dillon M, Hanukoglu I, et al. (1995). "Exclusion of the locus for autosomal recessive pseudohypoaldosteronism type 1 from the mineralocorticoid receptor gene region on human chromosome 4q by linkage analysis". J Clin Endocrinol Metab. 80 (11): 3341–5. doi:10.1210/jcem.80.11.7593448. PMID 7593448.
- ^ Chang SS, Grunder S, Hanukoglu A, Rösler A, Mathew PM, Hanukoglu I, et al. (1996). "Mutations in subunits of the epithelial sodium channel cause salt wasting with hyperkalaemic acidosis, pseudohypoaldosteronism type 1". Nat Genet. 12 (3): 248–53. doi:10.1038/ng0396-248. PMID 8589714. S2CID 8185511.